C. T. Holmes1, N. Clarke1, L. Powell1, M. E. Jessen1, M. Peltz1 1University Of Texas Southwestern Medical Center,Department Of Cardiovascular And Thoracic Surgery,Dallas, TX, USA
Introduction: Coronary artery bypass grafting remains the standard of care for treatment of multivessel coronary artery disease, particularly in diabetic patients. The influence of diabetic therapies on myocardial substrate selection under these conditions are unknown but may be important to ensure optimal outcomes after cardiac surgery. We hypothesized metformin and insulin alter myocardial substrate selection during cardiac surgery and may effect reperfusion cardiac function.
Methods:
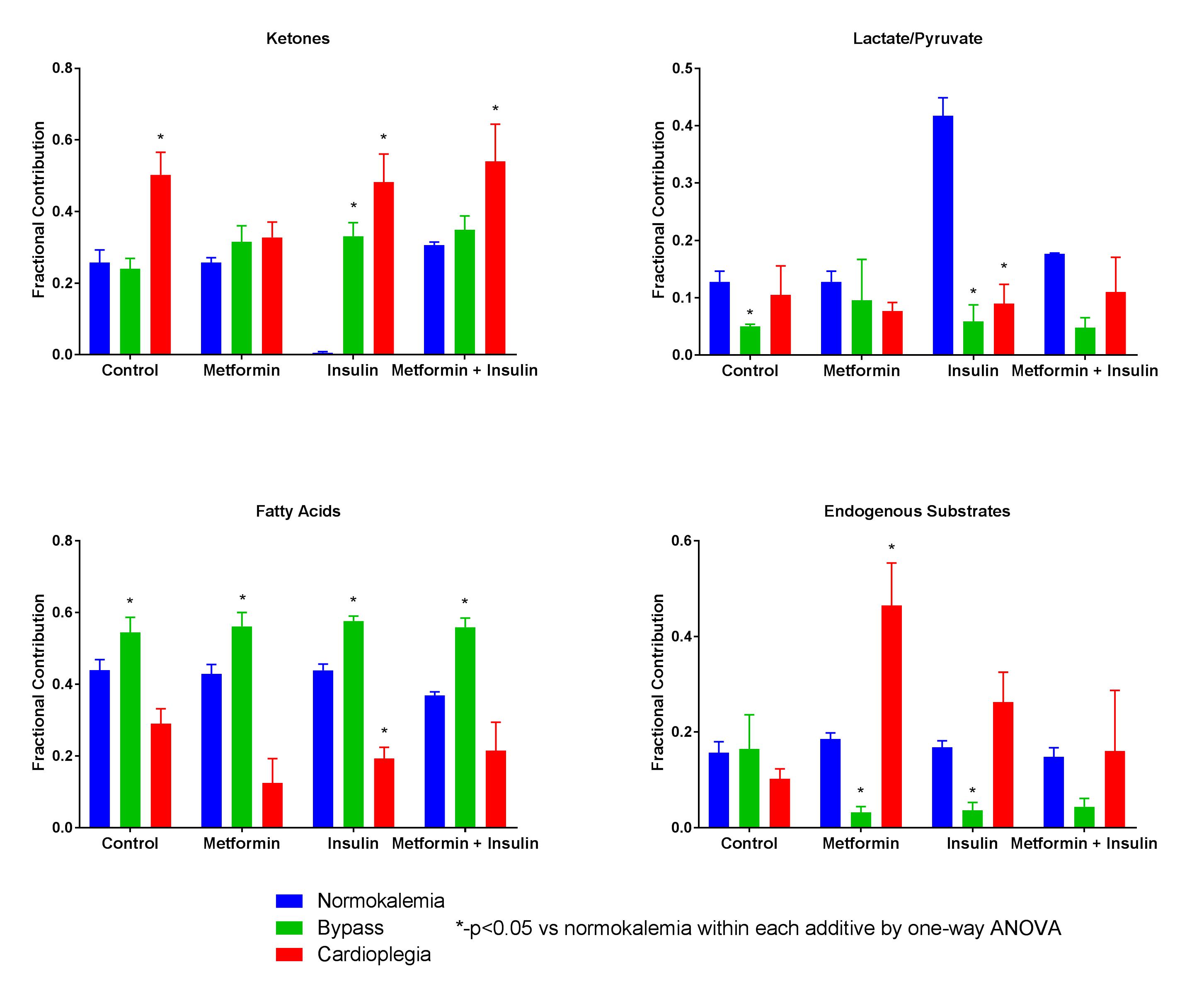
Groups of rat hearts (n=4 per group) were perfused under 3 conditions: Normokalemia, Cardioplegia or Bypass. Normokalemia groups were perfused with Krebs-Heinseleit buffer in the presence of no additives (Control), 500mM metformin (Metformin), 10 units/L insulin (Insulin), or both insulin and metformin (Metformin + Insulin). Cardioplegia animals were perfused with the same additives for 30 minutes with potassium modified buffer (20mM) to simulate cardioplegic arrest. Bypass groups containing the same additives were treated with three 22-minute ischemic intervals followed by a 3-minute interval of perfusion with cardioplegia buffer and 30 minutes of normokalemic reperfusion to simulate conditions encountered during coronary artery bypass grafting. Perfusion buffer with physiological concentrations of fatty acids (.35mM), ketones (.17mM), lactate (1.2mM), pyruvate (.12mM), and glucose (5.5mM) with different Carbon-13 (13C) labelling patterns was used for all conditions. 13C NMR spectra were obtained. Fractional substrate oxidation was determined by glutamate isotopomer analysis . Myocardial efficiency (rate*pressure/oxygen consumption) was measured in Bypass groups. Groups were compared by one-way analysis of variance or t-tests.
Results:
During cardioplegia, fatty acid oxidation was decreased for all additives. Ketone oxidation in this condition was increased with all additives except for metformin. Fatty acid oxidation was increased in all groups with a corresponding decrease in endogenous substrate oxidation when additive was included in the perfusion buffer. See Figure. Myocardial efficiency was not different for each additive compared to the stabilization period.
Conclusion:
Conditions encountered during cardiac surgery result in alterations in myocardial substrate oxidation profiles resulting in a reduction in fatty acid oxidation during potassium cardioplegia but increased fatty acid oxidation after reperfusion. These alterations in substrate oxidation did not affect myocardial efficiency in otherwise normal hearts.