C. Fiechter1, 2, K. Scheurlen1, A. Littlefield1, T. Alfieri1, S. Galandiuk1 1Price Institute of Surgical Research, Division Of Colorectal Surgery, Hiram C. Polk Jr. Department Of Surgery, University Of Louisville School Of Medicine, Louisville, KY, USA 2University Of Louisville, School Of Medicine, Louisville, KY, USA
Introduction: The incidence of early-onset colorectal cancer (EOCRC) (<50 years of age) has been steadily rising, while the prevalence of obesity is increasing among developed countries. Inflammation is a central pathophysiological mechanism in both CRC and obesity. Tumor-associated macrophages (TAMs) and the obesity-related hormones leptin and adiponectin mediate inflammation and affect tumor progression in CRC. Current evidence shows that anti-inflammatory M2-like TAMs are associated with tumor progression and worse patient prognosis in CRC. The macrophage-specific metabolite itaconate is produced by the enzyme Aconitate Decarboxylase 1 (ACOD1) in certain macrophage subtypes and is carcinogenic. The effects of obesity-related hormones and itaconate on cellular metabolism in CRC, however, are largely unknown. The aim of this study was to investigate inflammatory responses and the role of itaconate in TAMs and colon cancer cells using an in vitro co-culture model.
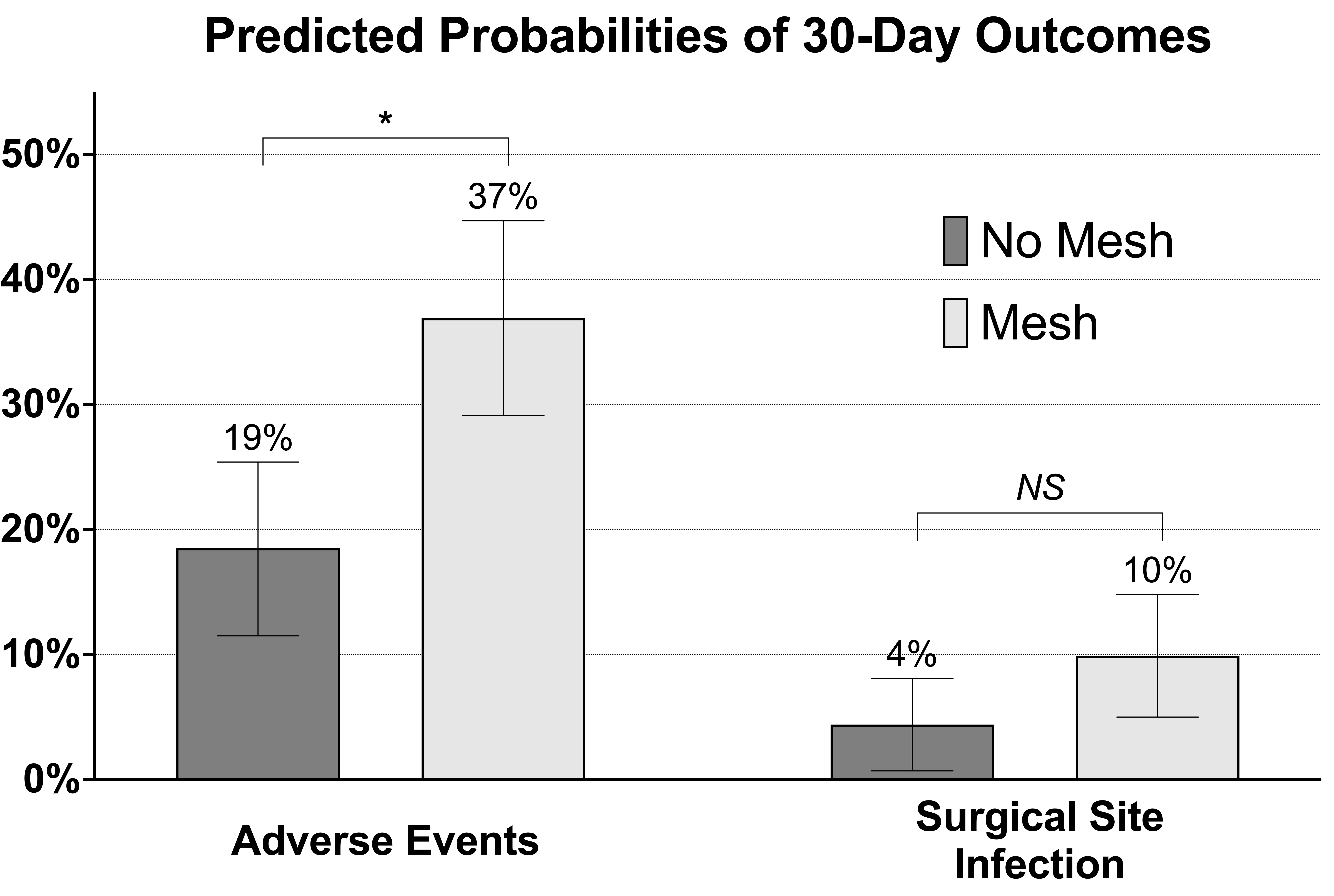
Methods: THP-1 monocyte cells were seeded into 24-well co-culture plates and polarized into M2-like macrophages within 14 days. Cells were then co-cultured with HT-29 colon adenocarcinoma cells and treated with either leptin, adiponectin, 4-octyl itaconate (OI) or dimethyl itaconate (DI) for 3 and 6 hours. Gene expression was analyzed using TaqMan qRT-PCR. Statistical analysis was performed using a Student’s t-test.
Results: In M2-like macrophages, proinflammatory IL-1β expression was significantly upregulated following adiponectin (30-fold, p=0.014) and leptin treatment (6-fold, p=0.026) for 6 hours (Fig. 1A). Expression of ACOD1 in M2-like macrophages was upregulated with adiponectin treatment (50-fold, p=0.002) for 6 hours (Fig. 1B). In HT-29 cells, OI treatment resulted in decreased expression of the proinflammatory cytokine CXCL10 at 3 hours (-5 fold-regulation, p=0.045) (Fig. 1C).
Conclusion: Adiponectin and leptin treatment results in a proinflammatory cellular response in TAMs, while the production of the carcinogenic and anti-inflammatory metabolite itaconate is induced. Therefore, the obesity-related hormones leptin and adiponectin activate tumor promoting mechanisms in CRC. Furthermore, the itaconate derivative OI decreases proinflammatory CXCL10 expression in colon cancer cells, thereby likely enhancing mechanisms of tumor growth and metastasis. In summary, the effects of adiponectin and leptin on M2-like TAM metabolism and cytokine expression in colon cancer may provide a link between obesity, inflammation and EOCRC.
C. N. Cook1, 2, K. Scheurlen1, J. George1, A. Swearingen1, S. Galandiuk1 1Price Institute of Surgical Research, Division Of Colorectal Surgery, LOUISVILLE, KY, USA 2University Of Louisville, School Of Medicine, Louisville, KY, USA
Introduction:
The incidence of early-onset colorectal cancer (EOCRC), diagnosed before the age of 50, has steadily increased during the last two decades, and approximately 80% of these cancers are sporadic. Obesity is also on the rise within the United States, and a possible link between metabolic dysfunction, inflammation and EOCRC has been suggested.
Within the tumor microenvironment, tumor-associated macrophages (TAMs) are able to regulate inflammation and to produce the anti-inflammatory carcinogenic macrophage-metabolite itaconate. While anti-inflammatory mechanisms and low peroxisome proliferator-activated receptor γ (PPARγ) expression in CRC are associated with advanced tumor stage and progression, the effects of itaconate on cellular metabolism and cancer progression are largely unknown. The aim of this study was to investigate carcinogenic cytokine expression and PPARγ levels in response to treatment with the macrophage-metabolite itaconate in human colon cancer cells.
Methods:
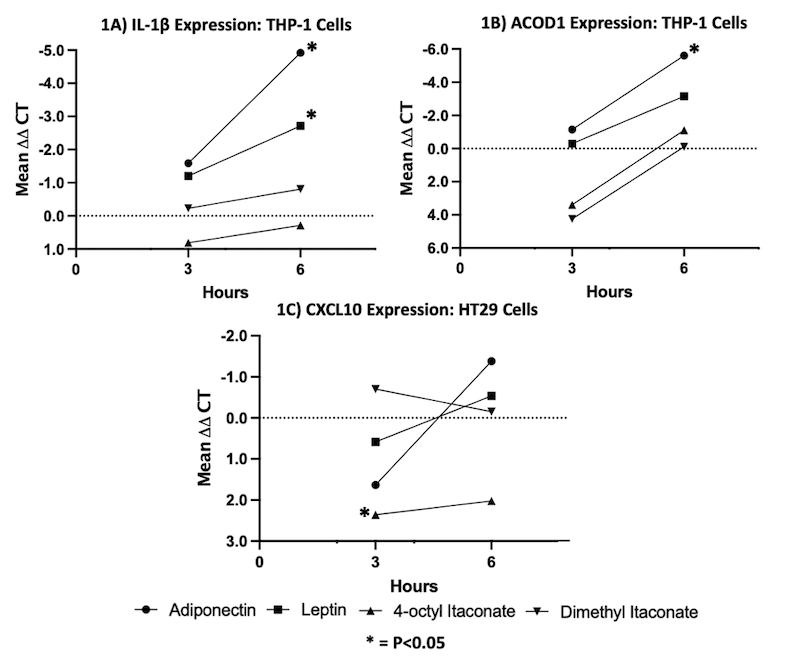
HT29 colon adenocarcinoma cells were plated into 24-well plates and rested for 24 hours. Cells were treated with the itaconate derivatives dimethyl itaconate (DI) or 4-octyl itaconate (OI) over four different incubation periods. Cellular mRNA was harvested, and qRT-PCR was performed, comparing cytokine and transcription factor gene expression in treated cells with untreated control cells resting in cell medium only. Statistical significance was evaluated using a paired t-test and results p<0.05 are displayed.
Results:
Dl downregulated expression of the proinflammatory cytokine IL-1β at 18 hours (-12-fold p=0.007) (Fig.1A). Proinflammatory CXCL10 was downregulated following DI treatment as well at 6 hours (- 3-fold p=<0.001),18 hours (-10-fold p=0.001) and 24 hours (-7-fold p=0.011) (Fig. 1B), respectively, which can promote tumor development. OI downregulated the transcription factor PPARγ in HT-29 colon cancer cells significantly after 6 hours (- 4-fold p=0.009), 18 hours (-4-fold p=0.004) and 24 hours (-8-fold p=<0.001) (Fig. 1C) of treatment, which is an expression pattern associated with worse outcome in CRC.
Conclusion:
Both itaconate derivatives, DI and OI, induce anti-inflammatory and carcinogenic effects in human colon cancer cells. While DI shifts cytokine expression in colon cancer cells towards a more anti-inflammatory profile, OI directly affects expression of a prognostically relevant transcription factor in CRC. We believe that TAMs mediate cancer-promoting mechanisms through an anti-inflammatory environment and PPARγ downregulation through itaconate in human colon cancer. Macrophage metabolism and itaconate production may link metabolic dysfunction and tumor development in patients with EOCRC.
M. A. Parks1, 2, K. Scheurlen1, D. Snook1, C. Seraphine1, S. Galandiuk1 1Price Institute of Surgical Research, Division Of Colorectal Surgery, Louisville, KENTUCKY, USA 2University of Louisville, School Of Medicine, Louisville, KENTUCKY, USA
Introduction: Early onset colorectal cancer (EOCRC)(<50 years) is a growing cause of cancer-related deaths in the United States. Similarly, obesity rates continue to trend up. CRC progression is affected by inflammation mediated through tumor-associated macrophages (TAMs) of a largely anti-inflammatory M2-like phenotype, that is associated with worse CRC prognosis.
The impact of the adipokine adiponectin on M2-like macrophages and progression in CRC is poorly understood. Anti-inflammatory cytokine expression, downregulation of the transcription factor Peroxisome Proliferator Activated Receptor g (PPARγ) and upregulation of Nuclear factor-κB (NF-κB) are associated with advanced tumor stage and worse outcome in patients with CRC. The aim was to investigate the effects of adiponectin on tumor-promoting cytokines, transcription factors, and cell surface markers following adiponectin treatment in M2-like macrophages.
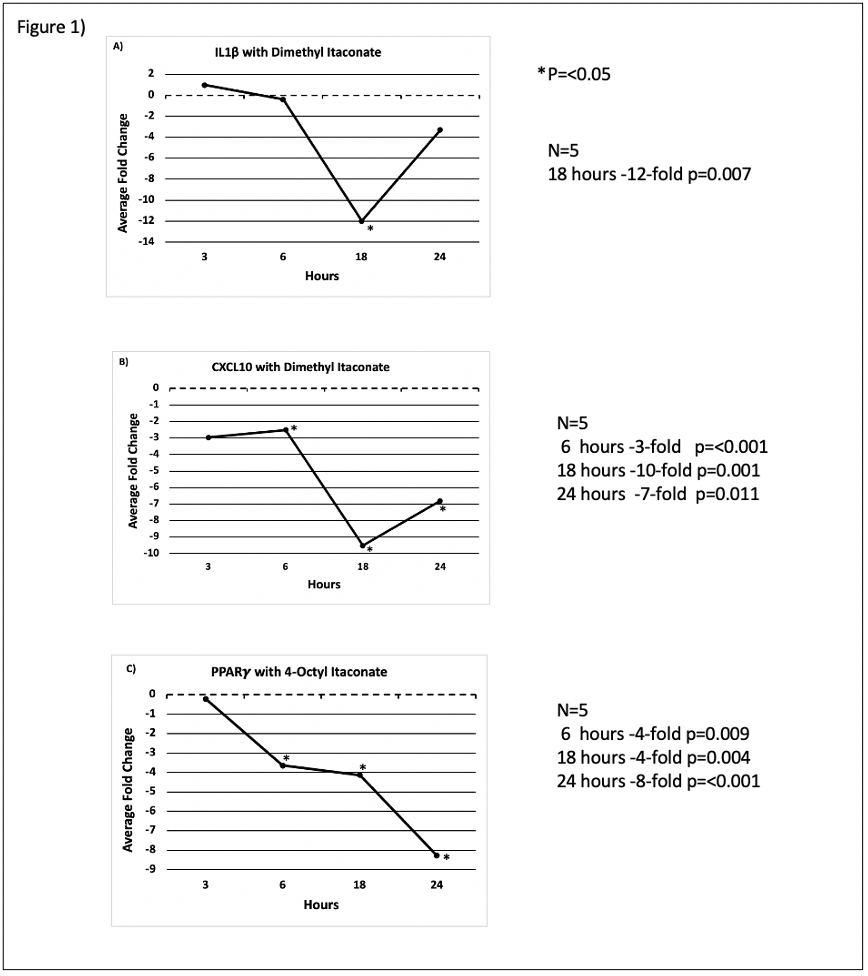
Methods: THP-1 cells were seeded onto culture plates and polarized into a distinct M2-like macrophage phenotype within 14 days. Cells were then treated with adiponectin for either 3, 6, 18, or 24 hours. mRNA was extracted and qRT-PCR was performed. Cytokine gene expression was measured relative to untreated control cells. For statistical analysis, paired t-tests were used.
Results: Following adiponectin treatment, M2-like macrophages showed a peak upregulation of the anti-inflammatory tumor-promoting cytokines C-C Motif Chemokine Ligand 22 (CCL22) after 24 hours (42-fold, p=0.002) and interleukin-8 (IL-8) after 18 hours (683-fold, p=<0.001), while IL-10 expression was maximally downregulated after 24 hours (- 9-fold, p=<0.001) (Fig. 1B). Peak upregulation of the tumor-promoting proinflammatory cytokines IL-6 (1130-fold, p=0.001) and IL-1b (485-fold, p=<0.001) was reached after 6 hours of adiponectin treatment, respectively (Fig. 1A). Expression of the M1-like macrophage surface marker CD80 was maximally increased after 6 hours (52-fold, p=0.003), while expression of the M2-like marker CD206 showed the lowest decrease at 24 hours (- 30-fold, p=<0.001) (Fig. 1C). NF-κB expression was increased at all time points with a peak at 6 hours (20-fold, p=<0.001) (Fig. 1D). We observed no significant change in expression of PPARγ or anti-inflammatory CCL18.
Conclusion: Adiponectin promotes expression of cancer-related cytokines and NF-κB in M2-like macrophages, thereby triggering cancer progression in CRC. Upregulation of the M1-like cell surface marker CD80 following adiponectin treatment shows that a phenotypic change of macrophages towards an M1-like proinflammatory phenotype is induced. Adiponectin may be an important a link between obesity, inflammation and EOCRC.
K. D. Feagins1, S. O’Brien1, T. Kalbfleisch2, H. C. Polk1, S. Galandiuk1 1University Of Louisville, Price Institute Of Surgical Research, Louisville, KY, USA 2University Of Kentucky, Gluck Equine Research Center, Lexington, KY, USA
Introduction: Familial adenomatous polyposis (FAP) is an autosomal dominant syndrome defined by APC gene mutations with numerous colonic adenomas developing early in life. Cancer risk is nearly 100% for FAP patients without intervention. The APC gene on chromosome 5q22 encodes a protein regulating Wnt signaling, ultimately functioning as a tumor suppressor.
Conversely, Crohn’s disease (CD) an inflammatory bowel disease with mechanisms not completely defined, is characterized by chronic inflammation and/or fibrostenotic strictures within the gastrointestinal tract. CD etiology is multifactorial; many genetic loci have been associated with CD and some (IBD5) are also on chromosome 5q.
We have identified a unique group of individuals with both disorders and hypothesize that there is an association between FAP and CD given the geographic proximity of IBD5 and APC on Chromosome 5.
We aim to:
1)assess the prevalence of previously identified cases of coexisting FAP and CD in the literature.
2)perform next generation sequencing (NGS) in dually diagnosed patients.
Methods: 1)We conducted a systematic review using the Preferred Reporting Items for Systematic Reviews (PRISMA). The PubMed, Embase, Ovid and Web of Science databases, dates from January 1950 to July 2020 were searched. A Google Scholar search was also performed. A search of grey literature was performed including Digestive Disease Week archives from 1974-2020. Relevant datapoints were extracted for descriptive analysis.
2)Whole blood was obtained from 8 patients with both FAP & CD after obtaining informed consent. NGS was performed, reads produced were mapped to the human reference genome build 38 at an average depth of coverage of 20X with paired end 150 base read length.
Results: Initial search yielded 1,214 articles. Inclusion criteria included full-text articles presenting coexisting/sequential cases of both FAP and CD. After titles and abstract screening, 1,120 articles were excluded with 94 selected for full text assessment; 12 were selected for systematic review, each describing patients with FAP and CD.
In our institution, we identified 4 cases of FAP associated with CD. NGS analysis showed each of these patients who are phenotypically similar to share the same genetic mutation; an 11 KB deletion in promoter 1B of the APC gene.
Conclusion: A systematic literature review yielded an additional 8 cases phenotypically similar to ours. Some articles include a comprehensive description of genetic data with little phenotypic detail. Conversely, other articles are clinical reports, without a genetic analysis. We have confirmed an 11KB APC promoter deletion in individuals with coexisting FAP and Crohn’s disease. Due to the infrequency of this mutation, and the co-occurrence of these conditions, further study may provide additional information regarding the etiology of Crohn’s disease in these patients.
M. G. Smithson1, R. Irwin1, G. Williams1, M. C. McLeod1, S. Bellis2, K. Hardiman1 1University Of Alabama at Birmingham, Surgery, Birmingham, Alabama, USA 2University Of Alabama at Birmingham, Cell, Development, And Integrative Biology, Birmingham, Alabama, USA
Introduction: Rectal cancer affects more than 44,000 patients annually. Traditionally, rectal cancer is treated with chemotherapy, radiation, followed by surgery but response to this treatment is variable. ST6Gal-1 is an enzyme that adds sialic acid (SA) to cell surface proteins and can modify function. Our previous studies have shown that ST6Gal-1 mediates resistance in rectal cancer cell lines, although the mechanism is poorly understood. We hypothesized that ST6Gal-1 increases following chemoradiation in primary rectal cancer organoids similar to what we have found in cell lines and that the mechanism of resistance is via decreased apoptosis.
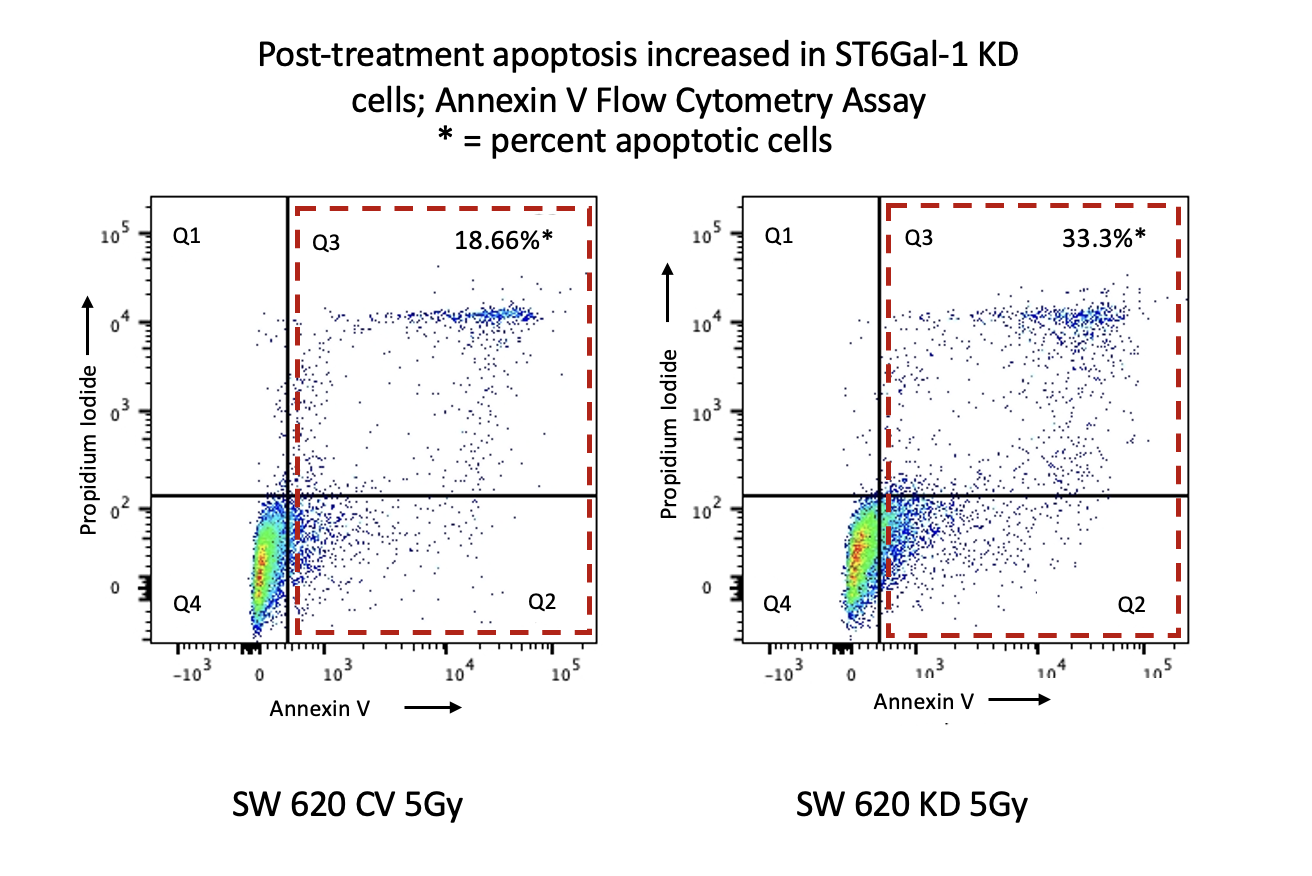
Methods: We assessed ST6Gal-1 in treated rectal cancer organoids made from patient tumor biopsies using fluorescent staining and PCR. SW620 cells were transduced with lentivirus containing shST6Gal-1 to knockdown the mRNA (KD) or an shRNA control vector (CV). Flow cytometry was used to assess Annexin V as a measure of apoptosis. SNA is a lectin which recognizes sialic acid placed on proteins by ST6Gal-1. An SNA Lectin pulldown was performed, and western blotting was used to assess for TNFR1 antibody.
Results: We treated primary rectal cancer with chemoradiation and assessed for ST6GaL-1. We found that ST6Gal-1 protein increased via immunofluorescent staining and PCR revealed a 3-fold increase in ST6Gal-1 mRNA on day 5 (N=3, p=0.007). To further explore mechanism, flow cytometry was performed in SW 620 rectal cancer cells following chemoradiation and identified 33.3% apoptotic cells in the KD group compared to 18.66% in CV cells containing ST6Gal-1. TNFR1, which has previously been shown to be sialylated, was also explored as a potential target. Cells underwent SNA lectin pulldown to collect sialylated proteins and found sialylated TNFR1 increased 2.91-fold in treated CV samples compared to untreated but this difference was not seen in KD samples.
Conclusion:
We have shown that ST6Gal-1 is increased in cell lines and rectal cancer organoids after chemoradiation, and that apoptosis is likely one mechanism mediating this resistance via TNFR1 sialylation.
B. W. Padon1, 2, T. J. Prajapati1, 2, F. M. Faruk1, 2, W. D. Short1, 2, O. Olutoye1, 2, H. Li1, 2, M. Rae1, T. Lu1, S. G. Keswani1, 2, S. Balaji1, 2 1Baylor College of Medicine, Pediatric General Surgery, Houston, TX, USA 2Texas Children’s Hospital, Pediatric General Surgery, Houston, TX, USA
Introduction:
Our lab has shown a significant role for IL-10 overexpression in regulating inflammation and extracellular matrix (ECM) production, thereby attenuating fibrosis in skin wounds. However, the role of IL-10 in wound closure is unclear, as previous studies in murine wounds, not controlled for contraction and moist wound environment, have shown increased rates of wound closure in IL-10-/- mice. The objective of this study is to determine the role of endogenous IL-10 on wound closure when controlling for contraction and a moist wound environment.
Methods:
Full thickness 6mm wounds were made in C57B6/J WT and IL-10-/- mice and controlled for contraction using a silicone stent. A moist wound environment was provided by Tegaderm dressing. Wounds were serially photographed at 3, 5 and 7d, harvested at 7d and 30d post wounding, then examined for epithelial gap, granulation tissue, scar area(H&E), myofibroblasts(aSMA), and leukocyte(CD45) and macrophage content(F4/80). Data is mean+-SD, n=8-10 wounds/group/time; p-value by ANOVA.
Results:
In contrast to prior reports, unstented IL-10-/- wounds maintained in a moist wound environment showed no significant difference in epithelial gap at d7, but had an increase in granulation tissue (IL-10-/- 1.4+-0.6 vs WT 0.8+-0.4 mm2, p<0.01) compared to WT. Unstented IL-10-/- wounds exhibited a heightened inflammatory response, with an elevated % of CD45+ (IL-10-/- 28.9%+-14.1 vs WT 6.0+-2.7, p<.01) and F4/80+ (IL-10-/- 53.7%+-1.2 vs WT 28.3+-0.5, p<.01) cells/high power field(HPF). Upon stenting the wounds, no difference in epithelial gap and granulation tissue was seen. The increase in % of F4/80+ cells/HPF (IL-10-/- 21.3%+-3.6 vs WT 22.4+-5.4, p<.05) persisted in stented wounds. There was a marked increase in the % of CD45+ cells/HPF (IL-10-/-22.4%+-1.5 vs WT 13.6%+-1.7, p=ns) as well. aSMA showed abundant expression at the wound margins in all wounds, but stented wounds had more aSMA present in the granulation tissue compared to unstented wounds. IL-10-/- wounds had more aSMA staining in the wound bed than WT. However, analysis of the % of aSMA + cells/HPF showed no significant difference in the stented and unstented wounds. At d30, wounds in IL-10-/- mice had significantly larger scar area as compared WT in stented (IL-10-/- 0.24+-0.02 vs WT 0.17+-0.06 mm2, p<.05) and unstented (IL-10-/- 0.18+-0.01 vs WT 0.13+-0.03 mm2, p<.05) groups.
Conclusion:
Our data showed endogenous IL-10 does not delay normal healing of skin wounds when controlled for contraction and moist environment. However, the loss of IL-10 leads to increased inflammation and fibrosis. This data signifies a previously unrecognized role for endogenously expressed IL-10 contributing to the tissue repair response.

A. Biswas1, H. J. Leraas2, S. Zadey2, P. Wilson3, B. Theriot4, N. Surana4, R. Ssekitoleko5, J. Mugaga5, C. Salzman1, A. Hall6, A. Saterbak1, T. Fitzgerald2 1Duke University, Biomedical Engineering, Durham, NC, USA 2Duke University, Surgery, Durham, NC, USA 3Duke University, Mechanical Engineering, Durham, NC, USA 4Duke University, Pediatrics, Durham, NC, USA 5Makerere University, Health Sciences, Kampala, Uganda 6Duke University, Pathology, Durham, NC, USA
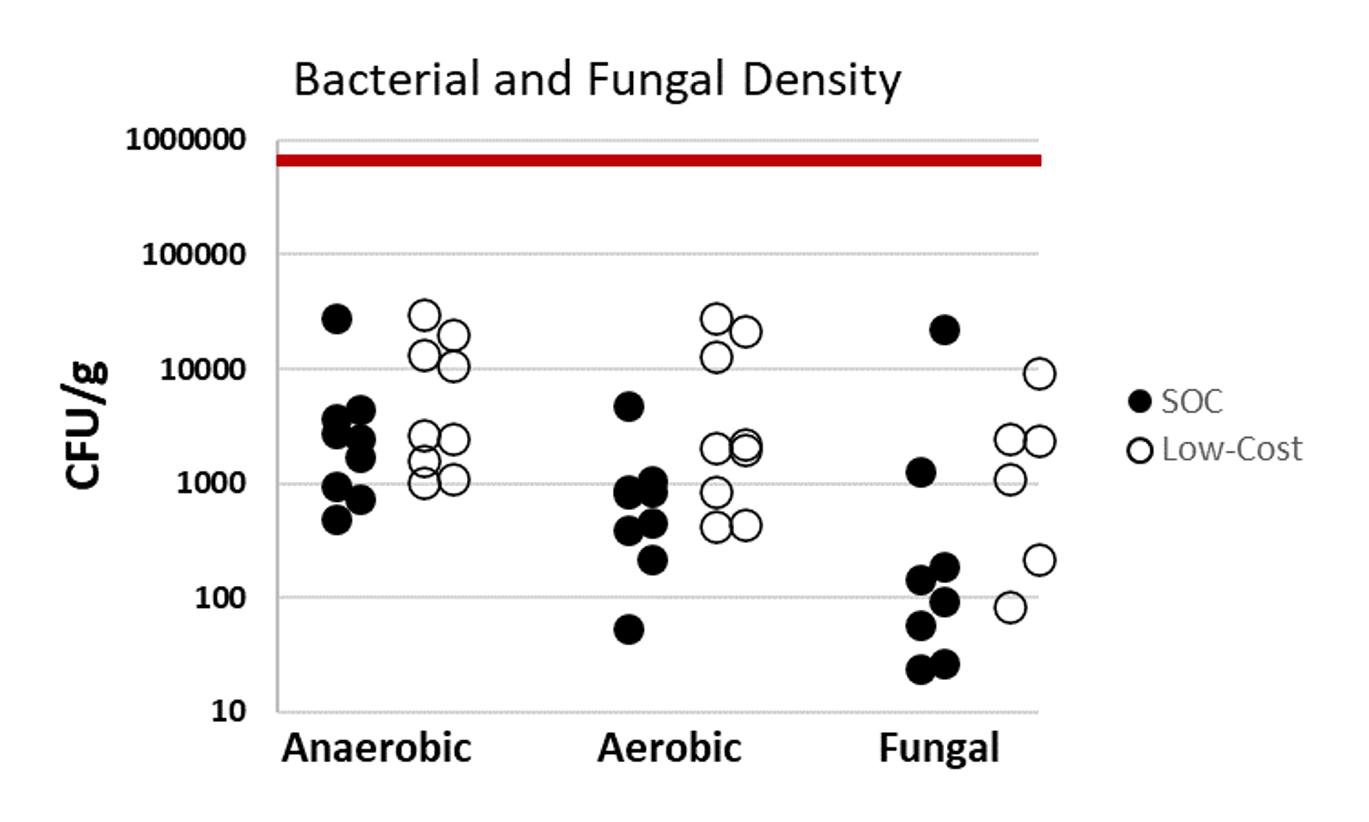
Introduction: Gastroschisis mortality in sub-Saharan Africa remains high at 59-100%. Silo inaccessibility contributes to this extreme disparity, as standard of care (SOC) silos cost $280, and most median family incomes in sub-Saharan Africa are <$200 per month. Our team of surgeons, engineers, and neonatologists from the U.S. and Uganda have previously described design and bench-testing of a low-cost (LC) silo that costs <$5 and is constructed from a urine collection bag and female condom ring, which are locally available in sub-Saharan Africa. Here we describe in vivo testing of the LC silos.
Methods: A piglet model of gastroschisis was achieved by eviscerating the intestines through a 2cm midline abdominal wall incision. The bowel was placed into either a LC or SOC silo, maintained for one hour and then reduced. Procedure times for placement, intestinal reduction and silo removal were recorded. Tissue injury was assessed by protocol-blinded histological examination of the abdominal wall and intestine. Quantitative assessment of bacterial and fungal growth on the silos were performed using standard culture techniques. Data were analyzed using the Mann-Whitney test (alpha=0.05).
Results: Six piglets (2.0-2.6 Kg) were block randomized to LC (n=3) or SOC (n=3) silo application. There was no visible gross injury to abdominal wall or intestine specimens in either the LC or SOC silos. Concurrently, there was no difference in minor bleeding (bruising) between the LC and SOC silos (Table 1). The differences in silo application times (LC 42 ± 48 seconds; SOC 47 ± 18 seconds; p=1.0), bowel reduction times (LC 6 ± 3.5 seconds, SOC 1 ± 2 seconds; p=0.40) and silo removal times (LC 2 ± 0.5 seconds, SOC 3 ± 1.5 second; p=0.40) between groups were not statistically or clinically significant, indicating similar ease of use. Microbiology analysis revealed bacterial growth on all samples, but the bacterial density was below the standard inoculum in vitro acceptability of 105 CFU/g for both the LC and SOC silos (Fig 1). There was no statistically significant difference in bacterial or fungal growth between the LC and SOC silos (anaerobic p=0.34; aerobic p=0.06; fungal p=0.80).
Conclusion: A low-cost silo, designed for manufacturing and clinical use in sub-Saharan Africa, demonstrated similar ease of use, absence of tissue injury, and acceptable microbiology profile similar to SOC silos. Data from this porcine model will allow our team to proceed with a pilot clinical study in Uganda.
S. A. Negash1, T. N. Mammo1, B. Ayele5, E. Anberber1, N. Starr4, T. G. Weiser2, 3 1Addis Ababa University, Surgery, Addis Ababa, ADDIS ABABA, Ethiopia 2University of Edinburgh, Surgery, Edinburgh, SCOTLAND, United Kingdom 3Stanford University, Surgery, Palo Alto, CA, USA 4University Of California – San Francisco, Surgery, San Francisco, CA, USA 5Addis Ababa University, Anesthesia, Addis Ababa, ADDIS ABABA, Ethiopia
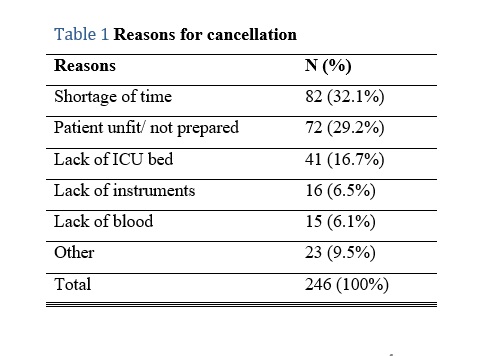
Introduction: The operating theatre is one of the most expensive areas of a hospital, requiring large capital and recurring investments, and necessitating efficient throughput to reduce costs per patient encounter. On top of increasing costs, inefficient utilization of operating theaters results in prolonged waiting lists, high rate of cancellation, frustration of OT personnel as well as increased anxiety that negatively impacts the health of patients. This problem is magnified in developing countries, where there is a high unmet surgical need. However, no system currently exists to assess operating theatre utilization in Ethiopia.
Methods: A prospective study was conducted over a period of 2 months (May-June 2018) at our hospital. It is the largest hospital in the country and has the highest number of operating theaters. Surgical case start time, end time, room turnover time, cancellations and reason for cancellation were observed to evaluate the efficiency of eight operating theaters.
Results: A total of 933 elective procedures were scheduled during the study period. Of these, 246 were cancelled, yielding a cancellation rate of 35.8%. The most common reasons for cancellation were related to patient preparation (29.2%) and shortage of time (32.1%). Lack of facilities accounted for 29.3% of cancellations. Start time was delayed in 93.4% of cases (mean 8:56 am + 52 min). First case completion time was early in 47.9 % and delayed in 20.6% (mean 2:54pm + 156min). Turnover time was prolonged in 34.5% (mean 25 min + 49 min). Total operating theater utilization ranged from 10.5% to 174%. Operating theaters were underutilized in 42.7% while overutilization was found in 14.6%.
Conclusion: We found a high cancellation rate, most of which are avoidable. The most common reason was shortage of time which could be associated with overbooking or inappropriate use of time due to other delays. Turnover time was longer than average, however, intervention in this area would likely not make an impact on efficiency as number of procedures per OT each day is low. Other measured causes of poor efficiency included late start of the first case and variable (very early or late) end of the last case. We recommend future quality improvement projects focusing on these two areas to increase OT efficiency.
B. Price1, G. An1, C. Cockrell1 1University Of Vermont College Of Medicine / Fletcher Allen Health Care, Surgery, Burlington, VT, USA
Introduction: The natural history of volumetric muscle loss (VML), such as wounds of the type suffered from significant blast-injury, is healing via scar formation. The functional recovery of patients with VML would be greatly enhanced if the VML could be replaced with functional muscle instead of scar. We have performed simulation experiments with an agent-based model of VML that have suggested a crucial tipping point in terms of scar formation versus muscle regrowth that is heavily influenced by the differentiation of fibroblasts to myofibroblasts. A review of the literature suggested an important role for α-smooth muscle actin (α-SMA) in the transformation of fibroblasts into myofibroblasts, and this prompted an in silico examination of the effect of inhibition of α-SMA accumulation on the ability to increase the muscle composition of a VML.
Methods: We have developed a mechanism-based agent-based model (ABM) to simulate the temporal evolution of a volumetric muscle loss (VML). Cells represented in the ABM include satellite stem cells, myoblasts, fibroblasts, and immune cell subtypes. Machine-learning techniques are used to develop a set of model parameterizations which encompass the biological heterogeneity seen clinically. Simulation experiments were performed that used Deep Reinforcement Learning (DRL) to incorporate the effects of inhibiting α-SMA accumulation along with other immunomodulatory controls to steer the system to maximize muscle in the healed wound.
Results: The DRL algorithm discovered treatment policies which increased the amount of functional muscle regenerated from 2% (in the untreated case) to 80% (when AI-controlled). The discovered therapeutic policy was complex, but upon examination, two primary objectives could be inferred: 1) control of inflammation such that muscle regeneration is not impaired, and 2) sufficient interruption of the differentiation of fibroblasts into myofibroblasts by inhibition of α-SMA accumulation, thus interrupting the conversion of granulation tissue to fibrotic scar.
Conclusion: In this work, we provide an in silico proof-of-concept study that demonstrates the importance of appropriate suppression of myofibroblast transformation in order to increase final wound muscle composition, and the need for a multi-modal intervention policy to accomplish this goal. These findings are a further demonstration of the utility of an integrated workflow that uses high-fidelity mechanism-based simulation with advanced machine learning and artificial intelligence to discover potential control strategies for complex pathophysiological processes.
T. J. Prajapati1, A. Kaul1, B. W. Padon1, 3, F. Faruk1, 3, W. D. Short1, 3, O. Olutoye1, 3, L. Yu1, 3, H. Li1, 3, O. Jung2, S. Jimenez2, J. Jung2, S. Balaji1, 3 1Baylor College Of Medicine, Pediatric General Surgery, Houston, TX, USA 2Louisiana State University, Biological Engineering, Baton Rouge, LA, USA 3Texas Children’s Hospital, Pediatric General Surgery, Houston, TX, USA
Introduction:
Impaired wound healing and scar formation have far-reaching socioeconomic effects. Excessive reactive oxygen species (ROS) cause oxidative stress in the wounds and delay healing by hampering vascularization and promoting inflammatory macrophage and myofibroblast differentiation resulting in increased inflammation and scarring. Engineered biomaterials capable of scavenging ROS and facilitating controlled release of oxygen can circumvent the challenge of oxygen diffusion in situ to promote cell infiltration and survival, which is not achieved with current biomaterials. We hypothesize that the application of novel lignin (an antioxidant from lignocellulose)-based composites with ROS-scavenging and oxygen-releasing properties will enhance neovascularization and attenuate inflammation to promote wound healing.
Methods:
We photo-crosslinked thiolated lignosulfonate (TLS) in methacrylated gelatin (GelMA) via thiol-ene chemoselective ligation. We developed calcium peroxide (CPO)-incorporated lignosulfonate/poly(lactic-co-glycolic acid) microparticles, where the dissociation of CPO into oxygen is facilitated by lignosulfonate, and added CPO particles to the GelMA-TLS composites and tested its antioxidant capacity (DPPH assay) and oxygen release (pseudo 1st order model). Full thickness 6mm wounds were made in C57BL/6N mice using silicone stents to control for contraction and divided into 4 groups: Untreated (UNTX), GelMA-TLS (TLS), GelMA-TLS with carriers but no oxygen release capacity (CPOc), and GelMA-TLS with carriers+oxygen release (CPO). Wounds were harvested at 7d and examined for epithelial gap, granulation tissue (H&E), myofibroblasts (αSMA), endothelial cells and vessels (CD31), and macrophages (CD206). Data presented as mean+-SD, n=3-6 wounds/group; p-value by ANOVA.
Results:
Morphometric wound analysis showed small differences in epithelial gap; however, treated wounds had greater granulating tissue area with marked increase in CPO (UNTX 1.9+-0.9 mm2 vs TLS 1.9+-0.8 vs CPOc 1.7+-0.4 vs CPO 1.5+-0.4, p<0.05). Notably, the CPO matrix was completely infiltrated and fully integrated with a granulating wound bed, unlike other groups which showed areas of non-infiltrated gel. CPO wounds had greater concentrations of αSMA in the middle of wound beds (UNTX 16.6+-8.7 % vs TLS 10.5+-8.7 vs CPOc 8.8+-2.4 vs CPO 17.5+-9.7, p=ns). Both CPOc and CPO wounds had greater vessel density (UNTX 14.0+4.7 lumens/40x field vs TLS 18.9+-3.9 vs CPOc 27.9+-7.2 vs CPO 25.2+-7.6, p<0.05). The CPOc and CPO wounds had fewer macrophages (UNTX 32.7+-12.4 % cells/40 field vs TLS 24.9+-14.3 vs CPOc 14.6+-4.4 vs CPO 19.3+-5.5, p<0.05).
Conclusion:
Our data demonstrates that the synergistic antioxidation and oxygen production capacity of lignin composites improved wound healing associated with reduced inflammation and enhanced neovascularization, representing new potential therapeutics for attenuating fibrosis and improving wound healing with engineered biomaterials.
S. S. Keswani1, 2, M. Potturu1, 2, S. Chawla1, 2, W. D. Short1, 2, O. Olutoye1, 2, S. G. Keswani1, 2 1Baylor College Of Medicine, Department Of Surgery, Houston, TX, USA 2Texas Children’s Hospital, Laboratory For Regenerative Tissue Repair, Houston, TX, USA
Introduction:
Women have begun to represent more of the surgical workforce, symbolizing continued success in promoting diversity, equality, and inclusion. Surgeons appointed to editorial boards, especially those of the main surgical journals, generally hold a moniker of high academic success in surgery. However, our prior data showed that there is a bias towards male editors in predominantly surgical journals. In this study, we sought to examine the degree of gender equality between different surgical subspecialties on the editorial boards of the major surgical journals.
Methods:
Surgical journals obtained from the Clairvate Web of Science Group Master Journals List were examined for editorial board composition. The surgical journal websites and faculty biography pages were used to determine the gender and educational background for each North American-based member of the editorial board, as well as the gender, educational background, and current academic title for each editor-in-chief. Individuals were further grouped by surgical subspecialty field. Statistical analysis was performed via t-tests and Chi-Square tests; significance was defined as p<0.05.
Results:
The composition of editorial boards based on gender was determined for 67 surgical specialty journals with impact factors ranging from 0.4 to 10.6. 2980 editorial board members were identified, with 593 (19%) female members and 2387 (81%) male members. When considering senior editorial board positions, only 9% of the 78 chief editors identified were female. The ratio of female members also varied by specialty – there was a significantly higher number of female senior editors in the non-surgical specialties (36%) compared to surgical specialties (13%, p<0.01). The top 4 surgical subspecialties to represent women on senior editorial boards were transplant surgery (20% female), general surgery (16%), otolaryngology/plastic surgery/ophthalmology (12%), and orthopedic surgery (10%). Furthermore, some fields had a higher number of female chief editors compared to the other subspecialties. For example, general surgery had the highest number of female chief editors (3), followed by surgical oncology (2) and cardiovascular surgery and transplant surgery (1). Interestingly, the average journal impact factor of female editors was higher than that of males (3.88 vs 2.88, respectively, p<0.05).
Conclusion:
Our analysis of the editorial board composition of surgical journals suggests there is variability in achieving gender equality amongst different surgical subspecialties and confirmed an overall bias towards male editors. Gender representation successes in non-surgical subspecialties and general surgery can be used to address equality issues in editorial leadership and shape a more diverse pool of surgeon scientists.
B. M. Tracy1, K. Nahum1, C. Paterson2, B. K. Poulose1, B. R. Hochman5, R. Rattan4, D. D. Yeh4, R. B. Gelbard3 1Ohio State University, Department Of Surgery, Columbus, OH, USA 2Emory University School Of Medicine, Department Of Surgery, Atlanta, GA, USA 3University Of Alabama at Birmingham, Division Of Acute Care Surgery, Birmingham, Alabama, USA 4University Of Miami, Department Of Surgery, Miami, FL, USA 5Columbia University College Of Physicians And Surgeons, Department Of Surgery, New York, NY, USA
Introduction: Antimicrobial guidance for common bile duct (CBD) stones during the perioperative period is limited. We sought to examine the effect of extended spectrum (ES) versus narrow spectrum (NS) antibiotics on postoperative outcomes in patients with CBD stones undergoing same admission cholecystectomy.
Methods: We performed a post-hoc analysis of a prospective, observational, multicenter study of patients undergoing same admission cholecystectomy for choledocholithiasis (CDL) and/or gallstone pancreatitis (GSP) between 2016 and 2019. We excluded patient with cholangitis, bacteremia, pneumonia, and/or urinary tract infections on admission; patients with perforated cholecystitis intraoperatively were also excluded. For both the pre- and postoperative periods, patients were divided into groups based on receipt of ES or NS antibiotics. Primary outcomes included surgical site infection (SSI) and/or severe sepsis. Secondary outcomes included hospital length of stay (HLOS) and acute kidney injury (AKI).
Results: There were 891 patients in the cohort; 49.9% (n=445) patients preoperatively and 21.2% (n=189) patients postoperatively received ES antibiotics. Patients receiving NS antibiotics during the preoperative period had significantly lower white blood cell counts on admission (8.7K vs 9.9K, p<.0001). There was no difference between groups regarding rates of SSI or sepsis in both the pre- and postoperative periods. However, patients receiving ES antibiotics postoperatively (5d vs 4d, p=0.002) had a longer HLOS. Rates of AKI were significantly higher for patients who received ES antibiotics in the preoperative (4.7% vs 2.0%, p=0.03) and postoperative (5.4% vs 0%, p=0.01) periods. For patients who received ES antibiotics during both the pre- and postoperative periods, the odds of AKI (OR 2.5, 95% CI 1.1-5.3, p=0.02) was significantly greater compared to NS antibiotics.
Conclusion: The incidence of SSI and severe sepsis were similar between patients treated with ES and NS antibiotics. However, the use of ES antibiotics was associated with a significantly longer HLOS and more than twice the risk of AKI. We caution the regular use of ES antibiotics in this patient population; however, randomized trials are needed to validate our findings.
S. Khedr1, A. Santos1, A. Torices Dardon1, K. Khariton1, C. Chen1, M. Kopp1 1NewYork-Presbyterian Queens, Surgery, Flushing, NEW YORK, USA
Introduction: Patient satisfaction is an important indicator of quality in healthcare and is linked to clinical outcomes, hospital rankings, patient retention, hospital reimbursement, malpractice claims, personal and professional satisfaction. Efficient physician-patient communication is essential to providing high-quality healthcare and improving patient satisfaction. Patients admitted to the hospital from the Emergency Department may not understand their diagnosis, reason for admission or plan of care, which can adversely impact their hospital experience and in turn reflect poorly in the Hospital Consumer Assessment of Healthcare Providers and Systems scores. We aim to identify risk factors that contribute to poor patient-physician communication.
Methods: From November 2020 to April 2021, patients admitted to the surgical floor were surveyed within 24 hours of admission. They were surveyed by either a Registered Nurse, Research Assistant, or Surgical Resident. They were asked “Do you know why you are in the hospital?”, “Do you know what your diagnosis is?”, “Do you understand your diagnosis?” and “Do you know what your treatment plan is?” A chart review was then performed recording patient demographics, preferred language, time of admission, health insurance, dependence in activities of daily living, dwelling, hearing impairment, pain level at time of admission, and number of chronic medical problems. Patients were excluded if they were < 18 years of age, had a history of neurocognitive disorders, had altered mental status defined as GCS < 15, required admission to the Intensive Care Unit or Step-Down Unit. Residents and attendings were debriefed regarding improving physician-patient communication at the end of January 2021 in order to raise awareness of the issue. Surveys answered before and after the brief intervention were compared.
Results: 131 patients that were admitted to the surgical floor were surveyed. Nineteen did not know their diagnoses (14%), 29 could not explain their diagnoses (22%), and 28 did not know their treatment plans (21%). A total of 29% of patients answered “no” to at least one question. Trauma patients (p = 0.027), patients with pain score > 4 at time of admission (p = 0.035), age > 65 (p = 0.044), and patients with >3 comorbidities (p = 0.035) were more likely to answer “no” to at least one of the questions. Limited English proficiency, insurance status, gender, and time of admission were not statistically significant barriers to effective communication. After raising awareness regarding improving physician-patient communication, we saw an 11% reduction in number of patients answering “no” to 24% from 35%.
Conclusion: Trauma patients, patients with poor pain control, the elderly and those with multiple comorbidities are more likely to experience poor patient-physician communication. Additionally, we found that raising awareness of the importance of this matter resulted in an improvement in communication.
D. Yun1, M. A. Plymale1, D. R. Oyler1, S. S. Slavova1, D. L. Davenport1, J. S. Roth1 1University Of Kentucky, College Of Medicine, Lexington, KY, USA
Introduction:
Previous research has shown nearly 1 in 2 ventral and incisional hernia repair (VIHR) patients have preoperative opioid use within a year before procedure. Development of new persistent opioid use after surgery is a valid concern, and the influence of preoperative opioid dose is not well known. The purpose of the study was to investigate the impact of preoperative opioid dose on postoperative opioid dose in a VIHR population.
Methods:
With IRB approval, a retrospective review of patient medical records was conducted on open VIHR consecutive cases (CPT codes: 49560, 49561, 49565, 49566) performed from August 2013 to July 2017 at a single institution. Kentucky All Schedule Prescription Electronic Reporting (KASPER) database was queried to obtain both preoperative and postoperative opioid use, dose, and prescription length. Preoperative opioid use was defined utilizing the CDC standard of any opioid use within 45 days prior to surgery, but data up to 90 days pre-admission and post-discharge was also analyzed. Morphine milligram equivalent (MME) was used for uniform comparison of dose among different prescriptions.
Results:
There were 235 patients who underwent VIHR during 2013 to 2017, and among them, 205 patients had KASPER record to extract opioid utilization data. Average age was 53.5 ± SD 12.0, and 50.7% were female. Over 35% met the criteria for preoperative opioid use, and the average MME level of 45 days in that group was 13.9 MME (90 day 14.1 MME). Among all patients, the postoperative 14-day opioid MME level was 693 (Opioid users 937, Opioid naïve 558, p < .001). Average 45-day MME of preoperative opioid correlated strongly with average 45-day MME of postoperative opioid use in patients who had mean ≥ 15 preoperative MME (r = .48, p< .001) but there was no correlation in patients with mean preop MME < 15 (r = .05, p = .643). 90-day MME of preoperative opioid also correlated significantly with 90-day postoperative MME (r = .673, p <.001).
Conclusion:
Preoperative opioid dose over both 45 and 90 days correlated strongly with postoperative opioid dose over the same timeframes for higher preoperative MME VIHR patients. Patients with average ≥ 15 MME 45-day preoperative opioid were likely to continue use at a similar level postoperatively, while lower MME patients were more arbitrary in their postoperative use. Further research exploring the indications of preoperative opioid use and its impact on postoperative opioid use in VIHR patients is needed.

E. George1, M. A. Olson2, S. Renshaw1, B. Poulose1 1The Ohio State University Wexner Medical Center, Department Of Surgery, Columbus, OHIO, USA 2Weill Cornell Medical College, Department Of Population Health Sciences, New York, NY, USA
Introduction:
The rates of chronic groin pain (CGP) after open inguinal hernia repair are reported between 18-51%. Previous literature has implicated nerve damage to be a significant factor and has increased awareness of proper nerve identification. However, the relative contribution of nerve management to CGP continues to emerge. Recent guidelines emphasize three-nerve recognition and handling (particularly iliohypogastric, ilioinguinal and genital branches of genitofemoral nerves) to minimize CGP. We sought to identify whether a strategy of three nerve identification (3N) and preservation results in decreased pain 6 months after open anterior inguinal hernia repair compared to two common strategies of nerve management: ilioinguinal nerve identification alone (1N) or two nerve identification (2N).
Methods:
We identified adult patients undergoing elective open anterior repair of unilateral inguinal hernias within the Abdominal Core Health Quality Collaborative (ACHQC). Six-month postoperative pain was defined using the pain domain of the EuraHS Quality of Life tool (range 0-30 with higher values indicating higher pain). A proportional odds model was used to estimate odds ratios and expected mean differences in 6 month pain for nerve management while adjusting for the logit of propensity score, baseline EuraHS pain score, and baseline confounders identified a-priori.
Results:
Between 2017-2021, 4451 patients were identified (358 (3N), 1731 (1N) and 2362 (2N) consisting mostly of White Non-Hispanic males (84%) over the age of 60, followed by African American males (8%) for both 3N and 1N groups and Hispanic males (9%) for 2N. The mean body mass index for each group was 26kg/m2. Academic centers identified all three nerves more often than ilioinguinal or two nerve identification methods. Median 6-month postoperative pain scores were 0 [IQR 0-2] for all nerve management groups (p = 0.51 3N vs 1N and 3N vs 2N). There was no evidence of a difference in the odds of higher 6 month pain scores in nerve management methods after adjustment (3N vs 1N OR: 0.95; 95% CI 0.36-1.95, 3N vs 2N OR: 1.00; 95% CI 0.50-1.85).
Conclusion:
While guidelines emphasize three nerve identification and preservation, the three nerve management strategies evaluated did not result in statistically significant differences in pain 6 months after operation. These findings suggest that nerve manipulation alone may not contribute as significant a role in CGP after open inguinal hernia repair compared to other factors.
B. K. Roberts1, 3, C. Nofi1, 3, M. Kobritz1, 3, L. Demyan1, 4, M. Giangola1, 2 1Northwell Health, General Surgery, New Hyde Park, NY, USA 2Zucker School of Medicine at Hofstra, New Hyde Park, NY, USA 3Feinstein Institute for Medical Research at Northwell, New Hyde Park, NY, USA 4Cold Spring Harbor Laboratory, Cold Spring Harbor, NY, USA
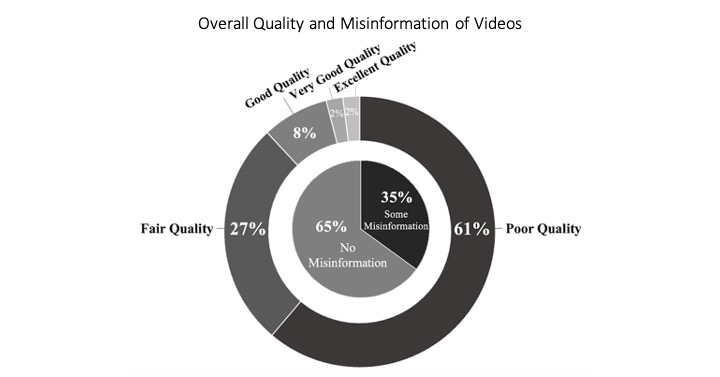
Introduction: With growing accessibility, patients are increasingly relying on social media for medical information. However, social media sources vary in quality and accuracy of patient information. Thus, utilization of social media may lead to misinformation regarding treatment for patients in need of emergent general surgery procedures.
Methods: YouTube was searched with keywords “cholecystectomy,” “cholecystitis,” and “gallbladder surgery” as well as “appendectomy,” “appendicitis” and “appendix surgery.” For each general surgical procedure, the 100 videos with the greatest total views were chosen for review. Videos were assessed by four surgical trainees using two validated instruments: DISCERN, a measurement of the quality of health information, and the Patient Education Materials Assessment Tool (PEMAT), a measurement of understandability and actionability of patient education materials. A Likert scale was used to estimate the amount of patient education and misinformation. Chi-square test was used, and statistical significance was set at p<0.05.
Results: The average number of views was 476,073 (93,670 to 7,976,292). The mean DISCERN score was 29.3 out of 75. The mean PEMAT scores were 64% for understandability and 22% for actionability. 49% of videos were rated as providing no patient education, while 29% provided some education and 22% provided a moderate level or more patient education. 35% of videos contained misinformation. The amount of misinformation was associated with type of video publisher; videos published by doctors, medical education and healthcare systems contained less misinformation, whereas videos published by patients, health/wellness groups contained more misinformation (p<0.001). Use of medical search terms “cholecystectomy” and “appendectomy” were associated with less misinformation (p<0.001, p=0.021). For counterpart colloquial searches, “gallbladder surgery” was associated with greater misinformation (p=0.001), whereas “appendix surgery” was not associated with misinformation.
Conclusions: There is a wide range of video quality that patients may use as resource for surgical information, with most videos being poor quality and providing little patient education. Although previous studies have shown that medical misinformation within social media exists, this study is the first to classify the scope of misinformation and quality of patient education related to emergency general surgery procedures. Understanding information available to patients online can help tailor surgeon-patient discussions to combat misinformation and improve the informed consent process for patients.
C. H. Lee1, R. Mabeza1, M. Park1, N. Chervu1, J. Hadaya1, K. Darbinian1, P. Benharash2 1David Geffen School Of Medicine, University Of California At Los Angeles, Surgery, Los Angeles, CA, USA 2David Geffen School Of Medicine, University Of California At Los Angeles, Cardiothoracic Surgery, Los Angeles, CA, USA
Introduction:
The Modified 5-point Frailty Index (mFI) has been incorporated in the National Surgical Quality Improvement Program (NSQIP) datasets as a means of identifying this condition in surgical patients. As frailty and colonic diverticular disease are both associated with advancing age, the study aimed to characterize the association of mFI score with clinical outcomes following colonic resections for diverticular disease.
Methods:
Adults (≥18 years) undergoing elective colon resection for diverticular disease were identified using the 2017-2019 NSQIP data reports. Subjects were assigned a point for each select comorbidity and grouped into 3 cohorts (mFI: 0, 1, >1). Prolonged length of stay (LOS) was defined as hospitalization longer than 95th percentile for the entire group. Multivariable regression analyses were used to examine the association of frailty with perioperative complications, unplanned reoperation, prolonged LOS, and 30-day readmissions.
Results:
Among 22,675 surgical patients with diverticular disease who met study criteria, 47% were in the mFI-1 and 1% in the mFI>1 group. Subjects with a mFI≥1 less frequently underwent laparoscopic vs open resection (75 vs 80%, p<0.001) and more likely to undergo colonic resection with stoma formation (7.1% vs 4.7%, p<0.001) compared to the mFI-0 group. Despite these differences, the operative times were similar among the mFI-0 and mFI≥1 groups (201±86 vs 191±81 minutes, p<0.001). After adjustment, frailty was associated with increased odds of perioperative complications and unplanned reoperation (Figure). With mFI-0 as reference, with each increase in mFI score groups, the odds for a prolonged LOS after the operation increased in a stepwise fashion (AOR 1.25 and 3.55, p<0.01) as did 30-day readmissions (AOR 1.26 and 1.74, p<0.05).
Conclusion:
With nearly half of patients undergoing colonic resections for diverticulitis carrying frailty defining comorbidities, this condition is associated with increased risk of complications, prolonged index hospitalization and 30-day readmissions. Preoperative assessment of frailty using the mFI may improve shared decision making and focus quality improvement efforts on this vulnerable cohort.
R. Mabeza1, C. Pan1, J. Hadaya1, M. Park1, C. Lee1, I. MacQueen1, P. Benharash1 1David Geffen School Of Medicine, University Of California At Los Angeles, Los Angeles, CA, USA
Introduction: Malnutrition has been associated with increased mortality and morbidity following various surgical procedures. However, its impact on outcomes following groin hernia repair has yet to be studied in a contemporary, national cohort. The present study aimed to assess the association of malnutrition with postoperative outcomes and resource use following groin hernia repair.
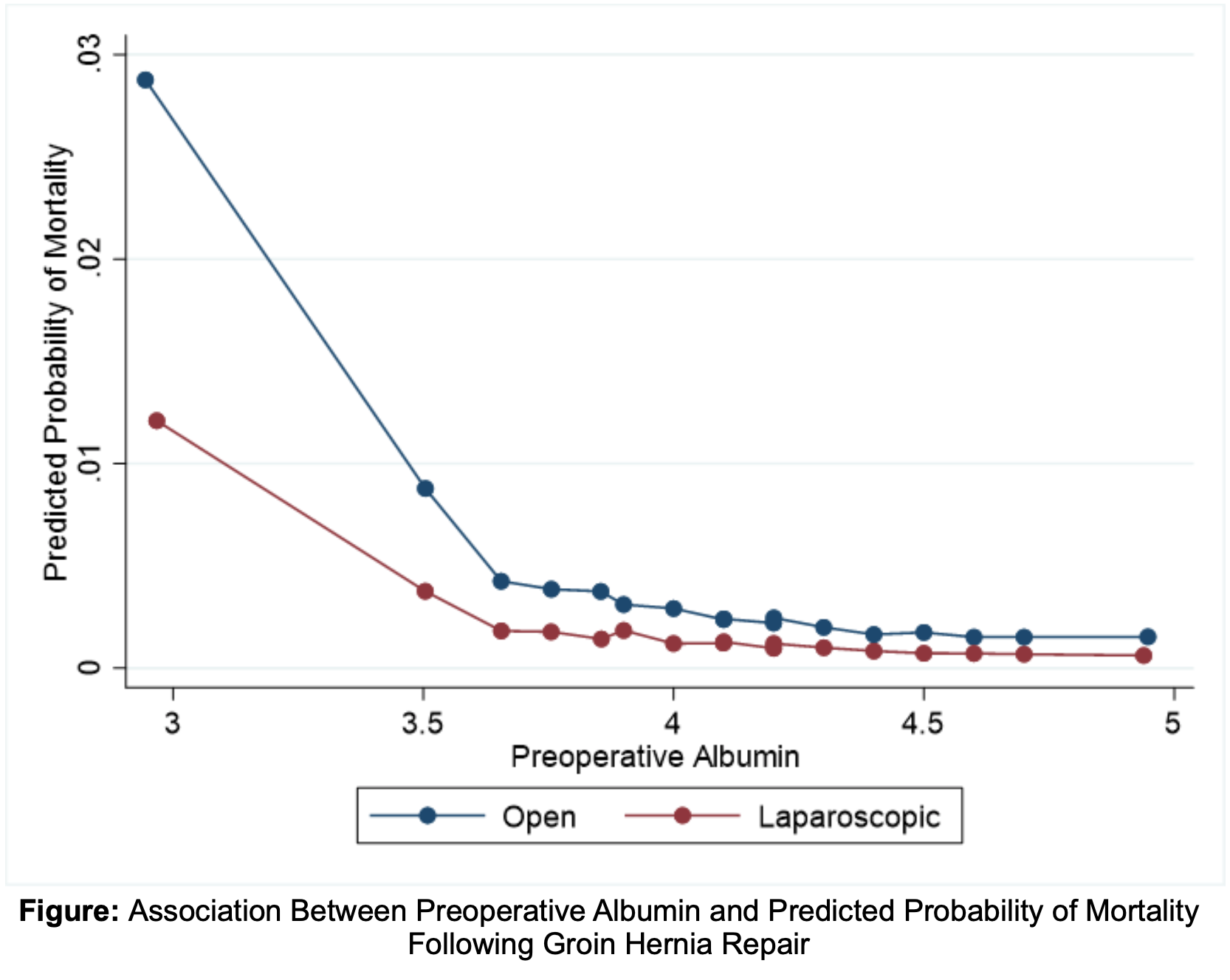
Methods: Adults (≥ 18 years) undergoing inguinal or femoral hernia repair (open and laparoscopic) were identified using the 2006-2019 American College of Surgeons National Surgical Quality Improvement Program Database. Patients with no recorded preoperative serum albumin were excluded. Malnutrition was defined as a preoperative albumin level < 3.5 g/dL. Multivariable regression models were developed to assess the association of malnutrition with outcomes of interest including 30-day mortality, complications (infectious, respiratory, and thrombotic), reoperation, postoperative length of stay (LOS), and readmission.
Results: Of the 106,555 patients meeting inclusion criteria, 8,002 (7.5%) were malnourished. Compared to others, malnourished patients were older (54.1 vs. 48.0 years, p<0.001), more commonly female (11.7% vs. 9.3%, p<0.001), and more frequently underwent an emergency (12.7% vs. 2.5%, p<0.001) or open procedure (82.5% vs. 66.6%, p<0.001). After risk adjustment, malnutrition was associated with greater odds of 30-day mortality (AOR 2.94, 95% CI: 2.30-3.77), infectious (AOR 1.71, 95% CI: 1.46-2.01), respiratory (AOR 2.07, 95% CI: 1.55-2.76), and thrombotic complications (AOR 1.72, 95% CI: 1.18-2.52). Additionally, malnutrition was associated with greater odds of readmission (AOR 1.79, 95% CI: 1.58-2.03) and increased LOS (β: +0.4 day, 95% CI: 0.3-0.4). Decreasing serum albumin levels were associated with increased probability of mortality for both open and laparoscopic hernia repairs, with significantly increased mortality at an albumin ≤ 3.5 (Figure).
Conclusion: Decreased preoperative serum albumin is associated with increased mortality and morbidity following open and laparoscopic groin hernia repair. Serum albumin remains a relevant predictor of postsurgical outcomes and can thus be used in counseling and shared decision making with malnourished patients in need of groin hernia repair.
L. M. Adams1, T. W. Costantini1, N. Neel1, A. E. Berndtson1, J. J. Doucet1, L. N. Godat1 1University Of California – San Diego, Division Of Trauma, Surgical Critical Care, Burns And Acute Care Surgery – Department Of Surgery, San Diego, CA, USA
Introduction: Surgical patients with acute and critical illness have an increased risk of venous thromboembolism (VTE). Trauma patients have high rates of VTE (7-9%) and are started on aggressive prophylaxis with twice daily enoxaparin administration and weight-based dosing; however, the optimal pharmacologic prophylaxis regimen in the emergency general surgery (EGS) patient has not been clearly defined. Patients with necrotizing fasciitis (NF) represent a group of EGS patients who typically present with severe illness associated with tissue injury and a heightened inflammatory state putting them at high risk for VTE. A better understanding of VTE risk for patients with NF is needed to guide clinical care. We hypothesize that the rates of VTE in patients admitted with NF will be high.
Methods: A retrospective review of the National Inpatient Sample database for the years 2017 & 2018 was performed for all patients >18 years old and admitted with an ICD10 diagnosis code for NF. Each admission was assessed VTE based on ICD10 codes for acute deep vein thrombosis and/or acute pulmonary embolism (PE). In addition, all patients were analyzed for surgical excision during hospitalization based on the ICD10 procedure codes for excision of skin, subcutaneous tissue, muscle, or fascia; those who didn’t have surgical excision were excluded from the analysis. For each patient we also obtained their age, sex, race, length of stay (LOS), insurance payer, hospital type, and mortality.
Results: There were 5168 patients admitted over the 2-year period with a diagnosis of NF. Of these patients 3280 (63.5%) were treated with surgical excision. For patients with NF treated with surgical excision, the mean age was 50.314.1 and 42.3% were female.
The overall VTE rate for patients treated with surgical excision was 3.1%; while 21.8% of these were an acute PE. In patients with VTE the LOS was significantly longer with a mean of 28.8 days (95%CI 24.0-33.7days) and in those without VTE 13.8 days (95%CI 13.3-14.3 days), p<0.001. The overall mortality rate for NF patients who underwent surgery was 13.5%; those with VTE had a significantly higher mortality rate at 30.7% (p<0.001).
Conclusion: Though the rate of VTE in patients with NF was low, the associated risk of PE and mortality was unexpectedly high. Further investigations with expanded clinical data are needed to better understand the risk of VTE in patients with NF. Close attention should be paid to ensuring timely VTE prophylaxis is administered, and high intensity regimens should be considered in these high-risk patients.
M. Katzen1, P. Colavita1, V. Augenstein1, B. Heniford1 1Carolinas Medical Center, GI & Minimally Invasive Surgery, Charlotte, NC, USA
Introduction:
ENT during adhesiolysis or SBR introduces contamination which may increase the risk of perioperative complications and thus hospital readmission. Given the cost and that readmission has become a significant quality metric, the aim was to evaluate nationwide patterns and outcomes of readmissions for patients who had an ENT or SBR during open ventral hernia repair (OVHR).
Methods:
The Nationwide Readmissions Database was queried between 2016-2018 for those with ICD-10-CM diagnostic code for ventral hernia and ICD-10-PCS procedure code for OVHR. Respective comparison groups were created using ICD-10 codes for ENT or SBR.
Results:
Over 3 years, 105,845 patients were admitted for OVHR. ENT occurred in 1202 (1.14% total OVHR) and 997 involved SBR (0.94% total OVHR). ENT was more common during elective procedures (1.2% elective vs 1.0% non-elective;p=<0.01) while SBR was more common during non-elective admissions (0.48%vs1.64%;p=<0.01).
Compared to OVHR without ENT or SBR, ENT and SBR groups were older (60.5 OVHR vs 62.0 ENT and 64.1 SBR; both p=<0.01). Mean Charlson Comorbidity Index was lowest in the ENT group and highest in the SBR group (1.34 vs 1.17 and 1.53;both p=<0.01). Smoking history was less common in SBR (12.5% vs 12.3% and 10.2%;p=0.83 and 0.03). Rates of diabetes were similar (24.2% vs 23.5% and 22.5%;p=0.61 and 0.21). ENT and SBR patients were less likely to be obese (31.7% vs 25.9% and 28.9%;p=<0.01 and 0.07). ENT patients had more readmission within 90 days after elective or non-elective primary admissions (elective: 16.2% OVHR vs 23.0% ENT,p=<0.01; non-elective: 19.4% OVHR vs 25.0% ENT,p=<0.01). SBR patients had the highest readmission rate but remained unchanged by elective/non-elective primary admission (26.2% vs 26.2%). ENT or SBR had longer median length of stay(LOS) (4 days OVHR vs 6 ENT and 8 SBR; both p=<0.01) and higher hospital charges ($34,790 vs $81,966 and $106,298;both p=<0.01). The most common readmission diagnosis was infection (33.0%OVHR vs 33.3%ENT and 34.8%SBR;p=0.90/0.55). ENT and SBR were more often readmitted for obstruction (7.3% vs 12.1% vs 10.7%;p=<0.01/0.04). There was no difference in reoperation for recurrence (4.9% vs 6.4% vs 3.5%;p=0.30/0.33), but ENT was more likely to have reoperation for obstruction (1.3% vs 5.3% vs 2.8%;p=<0.01 and 0.053). Logistic regression models demonstrated that ENT and SBR were independently associated with readmission (OR 1.33 ENT, 1.36 SBR).
Conclusion:
Compared to OVHR without ENT or SBR, both ENT and SBR are associated with longer LOS, increased charges, and higher readmission rates. OVHR with ENT or SBR was associated with higher rates of readmission and reoperation for obstruction, but no difference in readmission for infection.
B. N. Thompson1, S. L. Adkins1, K. Howe1, J. R. Gillen1 1Virginia Tech Carilion School of Medicine, Carilion Clinic, Department Of Surgery, Roanoke, VA, USA
Introduction:
The opioid epidemic has instigated widespread re-evaluation of opioid prescribing practices. The purpose of this study was to evaluate the impact of new electronic medical record (EMR) order sets on current general surgery opioid prescribing practices. We hypothesize that with implementation of standardized guidelines, a reduction in opioid prescribing can be achieved.
Methods:
This is a single institution prospective cohort study of patients ages 18-89 who underwent inpatient general surgery with length of stay (LOS) < 2 days between October 2018 and March 2021. Cohorts pre- and post- implementation of standardized postoperative EMR order sets in October 2020 were compared. Procedure specific guidelines for prescribed opioids in morphine milligram equivalents (MME) were recommended. Primary outcome assessed was discharge MME. Cohort comparisons were performed with Chi-square analysis. Threshold for significance was considered p<0.005 after Bonferroni adjustment.
Results:
There was no difference in baseline characteristics of pre- (n=5098) and post-intervention (n=1113) cohorts (Table 1). There was a significant reduction in discharge MME post intervention (70.11 vs 86.49, p<0.0001) without associated increase in opioid refills.
Conclusion:
Surgery patients represent a vulnerable population in the present opioid epidemic. Implementation of EMR order sets maximizing nonopioid analgesia was associated with decreased postoperative opioid utilization. Utilizing procedure specific opioid prescribing guidelines for outpatient general surgery can further optimize surgeon opioid prescribing practices.

M. Stawikowska1, 3, G. Toryn2, C. Marques2, M. Pansari1, M. Jacobs1, 3, S. Patil1, 3 3Michigan State University, College Of Human Medicine, Lansing, MI, USA 1Ascension Providence Hospital, General Surgery, Southfield, MI, USA 2American University of the Carribean, Medical School, Southfield, MI, USA
Introduction:
Perforated peptic ulcer is an acute surgical emergency and surgical intervention is the standard of care. However, in certain patients the risk of surgery outweighs its benefit, and they are simply better suited for conservative management. This current study compares the outcomes of surgical and conservative management of patients with a perforated peptic
ulcer.
Methods:
National Inpatient Database (NIIS 1998-2014) was used to identify patients admitted with a perforated peptic ulcer (ICD 531.10, 532.10). Standard statistical methods were used to evaluate demographic data and outcomes of patients who were treated conservatively or with surgery.
Results:
10,033 patients were admitted with an acute perforated peptic ulcer, with a M to F ratio 0.97:1. Mean age was 62.3±2 years. 58.8% of patients were Caucasian, 10.2% African American, 5.0% Hispanic and 2.7% Asian Pacific Islanders. 1,209 (12%) patients received no surgery, while 8,824 (88%) underwent surgery. Average age was 62.1±19.0 in surgery and 63.9 ±18.9 in no-surgery group. Surgery was the prevalent treatment across all races with no significant difference in treatment and discharge to home status. Nearly 55% patients in both groups were discharged to home. Mortality rate was 11.4% in surgery compared to 14.3% in no- surgery group, p <0.01. Surgical patients developed complications more commonly than no- surgery group, especially cardiac (4.1% vs. 1.0%) and respiratory complications (11.2% vs. 5.5%) were statistically significant, p <0.01. 83.9% of patients in rural hospitals underwent surgery, compared to 89.8% at urban non-teaching and 87.8% at urban teaching hospitals, p<0.01. The hospitalization cost and LOS was significantly higher in the surgical group, p<0.01.
Conclusion:
Surgery is the prevalent form treatment for perforated peptic ulcer, across allraces. Surgical intervention is less common in rural hospitals. Surgical intervention is associated with higher cardiac and respiratory complications, increased cost of care and LOS.
However, mortality rates were significantly higher in no-surgery group (14.3% vs. 11.40%). Further single institution studies are needed to validate these findings and provide treatment guidelines.

T. Efejuku2, J. Song1, A. Palackic1, S. E. Wolf1 1University Of Texas Medical Branch, Department Of Surgery, Galveston, TX, USA 2University Of Texas Medical Branch, School Of Medicine, Galveston, TX, USA
Introduction: The number of research publications produced is strongly correlated to academic promotion and tenure. That said, clinician-scientists report growing difficulty in balancing clinical duties with teaching, professional, and research obligations. The continued struggle presents the question of whether research productivity is quantitatively related to clinical activity. Our study aims to identify correlations, if any, of research publications and clinical performance benchmarks in academic surgical departments.
Methods: An electronic search was performed using SCOPUS to identify 14 Departments of Surgery in Texas academic institutions from 1970 to 2020. Texas was divided into three regions (Gulf Coast, West Texas, and Central/Northeast Texas) by geographic location and city population to equalize distribution. The number of published articles in 2019 was correlated to clinical activity for the same year obtained from the American Hospital Directory. The database lists statistics from hospitals in Texas in various categories including staffed hospital beds, total discharges, patient days, gross revenue, number of Medicare inpatients, average length of stay, average charges, and Medicare CMI. Pearson correlation analysis was utilized to compare number of publications to these clinical performance benchmarks.
Results: Data showed a steady increase in the total number of published articles from the 14 Texas institutions from 1970-2020. When stratified by the three regions for 2019, we found a strong negative correlation (r = -0.91) with the number of publications to sum of the average charges for clinical care. We also found a strong positive correlation (r = 0.87) between the total number of surgical publications in 2019 and the sum of the average length of stay. All other variables had weak or no correlation.
Conclusion: The strong negative correlation for number of publications and average charges per institution stands as the best indication that research productivity positively effects clinical activity, even among academic institutions. We also found that research productivity is correlated with increased average length of hospital stay as another clinical impact of increasing research effort. While surprising, such findings should be considered in strategic management of academic surgical institutions.
B. H. Jacobson1, J. Zheng2, E. J. Orav3, T. C. Tsai2, 4 1Stanford Medical School, Stanford, CA, USA 2Harvard T.H. Chan School of Public Health, Department Of Health Policy And Management, Boston, MA, USA 3Brigham And Women’s Hospital, Division Of General Internal Medicine And Primary Care, Boston, MA, USA 4Brigham And Women’s Hospital, Department Of Surgery, Boston, MA, USA
Introduction: Fragmentation of post-surgical care has been associated with an increased risk of mortality among surgical patients, but it is unknown how the overall health and vulnerability of patients – such as frailty – influences the potential harm that they face when receiving fragmented post-surgical care. We therefore assessed whether frail patients were especially vulnerable to increased mortality associated with fragmented post-surgical care.
Methods: Using Medicare inpatient claims data from 2005-2016, we examined a cohort of 221,225 surgical patients who underwent hip replacement, knee replacement, colectomy, coronary artery bypass grafting, or pulmonary lobectomy and were then readmitted following surgery. A multivariable logistic regression was used to assess whether higher odds of mortality were associated with frail patients receiving fragmented post-surgical care.
Results: 28% of patients in the sample were frail as defined by a validated claims-based index, and 25% were readmitted to a different hospital from the one where their surgery was performed. 30-day mortality was highest in frail patients with fragmented care (4.1%) and lowest in non-frail patients with unfragmented care (2.1%), and this remained true when examining risk-adjusted 30-day mortality. Fragmentation of care resulted in an equal adverse effect on 30-day mortality across both frail and non-frail patients (0.77% increase in mortality among frail patients, 0.75% increase in mortality among non-frail patients, p = 0.96).
Conclusion: Frail patients receiving fragmented post-surgical care were associated with nearly double the mortality of non-frail patients without fragmented post-surgical care, highlighting the additive effects of fragmentation and frailty on mortality. Given that fragmentation poses an additional burden to frail patients already facing increased post-surgical mortality, frailty pathways for surgical patients and geriatric centers of excellence should aim to reduce fragmented post-surgical care for frail patients in order to improve outcomes for this vulnerable patient population.

R. Howard1, Q. Solano1, L. Delaney1, B. Fry1, A. Ehlers1, M. Englesbe1, J. Dimick1, D. Telem1 1Michigan Medicine, Ann Arbor, MI, USA
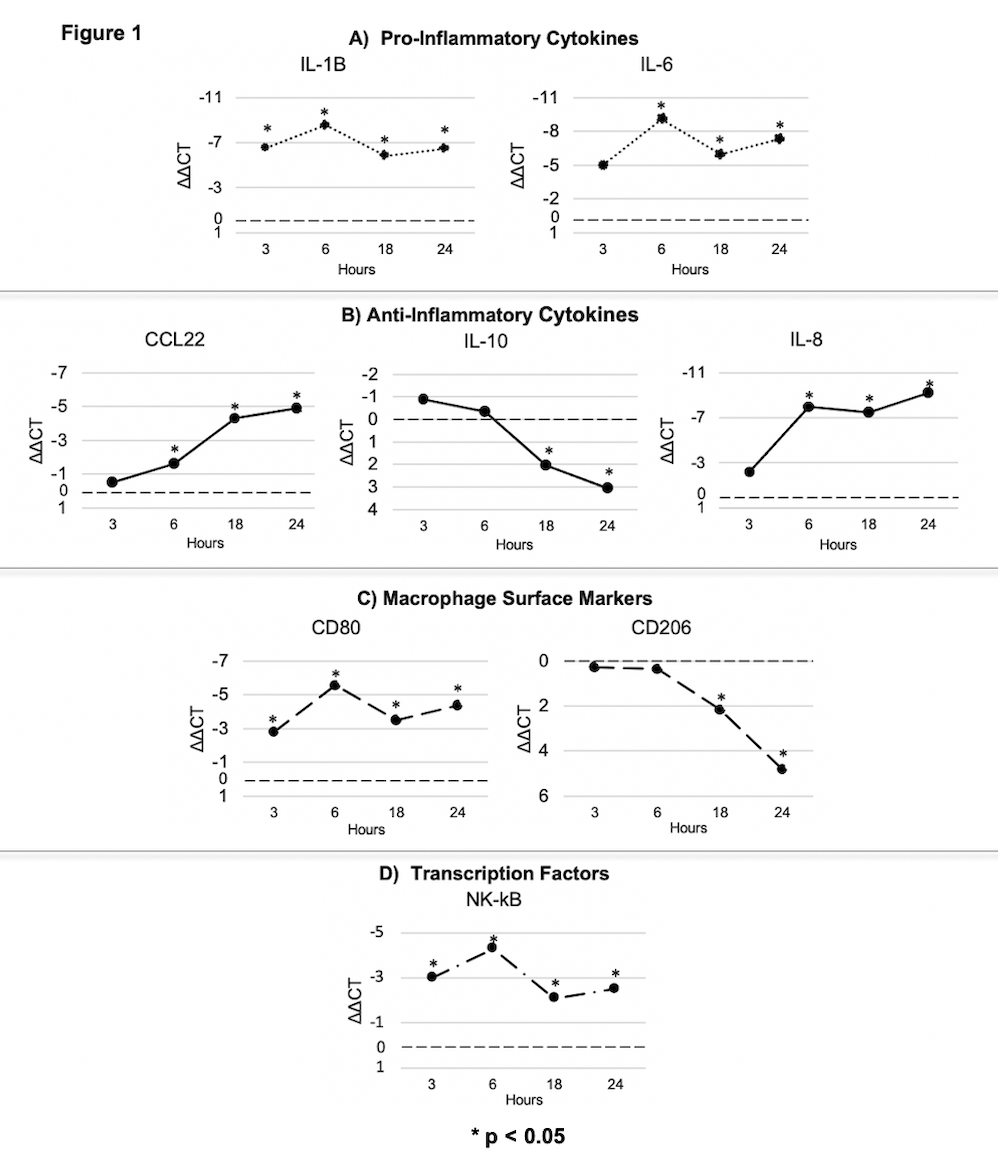
Introduction: Use of mesh in clean/contaminated and contaminated ventral hernia repair (VHR) is controversial. While longitudinal trials have shown that mesh reduces long-term hernia recurrence, other studies have raised concern over increased infectious complications when mesh is placed in a contaminated field. The impact of this conflicting evidence on real-world mesh use is also poorly understood. We conducted the following study to understand current practice and outcomes in mesh use for clean/contaminated and contaminated VHR.
Methods: We performed a retrospective review of the Michigan Surgical Quality Collaborative Hernia Registry (MSQC-HR), which is a novel, statewide clinical registry that captures granular hernia-specific variables such as location and mesh use for patients undergoing VHR. The study cohort was adult patients undergoing clean/contaminated and contaminated VHR between January 1, 2020 and July 1, 2021. The exposure of interest was use of mesh which was classified as permanent or absorbable. The primary outcome was a composite end point of 30-day adverse events including complications, emergency department use, readmission, and reoperation. The secondary outcome was surgical site infection (SSI). Multivariable logistic regressions accounting for patient, hernia, and operative characteristics were estimated to calculate the independent association of mesh use with 30-day adverse events and SSI.
Results: 275 patients underwent clean/contaminated and contaminated VHR performed by 152 surgeons at 49 hospitals. Mean age was 56.4 (13.9) years and 152 (55.3%) patients were female. Mesh was implanted in 169 (61.5%) patients and consisted of permanent mesh in 147 (87.0%) patients and absorbable mesh in 22 (13.0%) patients. 30-day adverse events occurred in 57 (33.7%) patients with mesh and 23 (21.7%) patients without mesh (P=0.033), whereas surgical site infection occurred in 16 (9.5%) patients with mesh and 5 (4.7%) patients without mesh (P=0.149). After adjusting for patient, hernia, and operative characteristics, mesh use was associated with higher odds of adverse events after surgery (aOR 2.83 [95% CI 1.48-5.41]), but was not associated with higher odds of SSI (aOR 2.57 [95% CI 0.81-8.10]) (Figure).
Conclusion: In this study of real-world mesh use in clean/contaminated and contaminated VHR, mesh was used in most patients and was almost exclusively permanent. Although mesh placement was not associated with increased odds of infection, it was associated with increased adverse events even after controlling for patient, hernia, and operative characteristics. This suggests that additional work using granular hernia-specific data is needed to understand how mesh use drives adverse events after surgery in this population.