E. A. Bailey1, C. E. Sharoky1, C. Wirtalla1, R. R. Kelz1 1Hospital Of The University Of Pennsylvania,Center For Surgery And Health Economics, Department Of Surgery,Philadelphia, PA, USA
Introduction: The link between mental and physical health is poorly understood. Patients with mental health disorders have worse oncologic and chronic disease management and experience excess mortality compared to those without a mental health comorbidity. This study aims to evaluate the relationship between mental health comorbidities and surgical outcomes.
Methods: We conducted a retrospective cohort study using the 2009-2011 National Inpatient Sample (NIS) database. All patients aged 18-90 who underwent one of the top four most common general surgery procedures (cholecystectomy, colectomy, small bowel resection/lysis of adhesions, and appendectomy) were included. Patients were classified as having a mental health diagnosis if they had a DSM IV diagnosis present on admission. Diagnosis categories included anxiety, mood, impulse control disorders, substance abuse, and schizophrenia. Descriptive statistics were performed. Multivariable regression examined post-operative outcomes including length of stay (LOS), in-hospital mortality, and complications while controlling for age, sex, race, admission status, non-mental health co-morbidities, insurance status, and income quartile by zipcode.
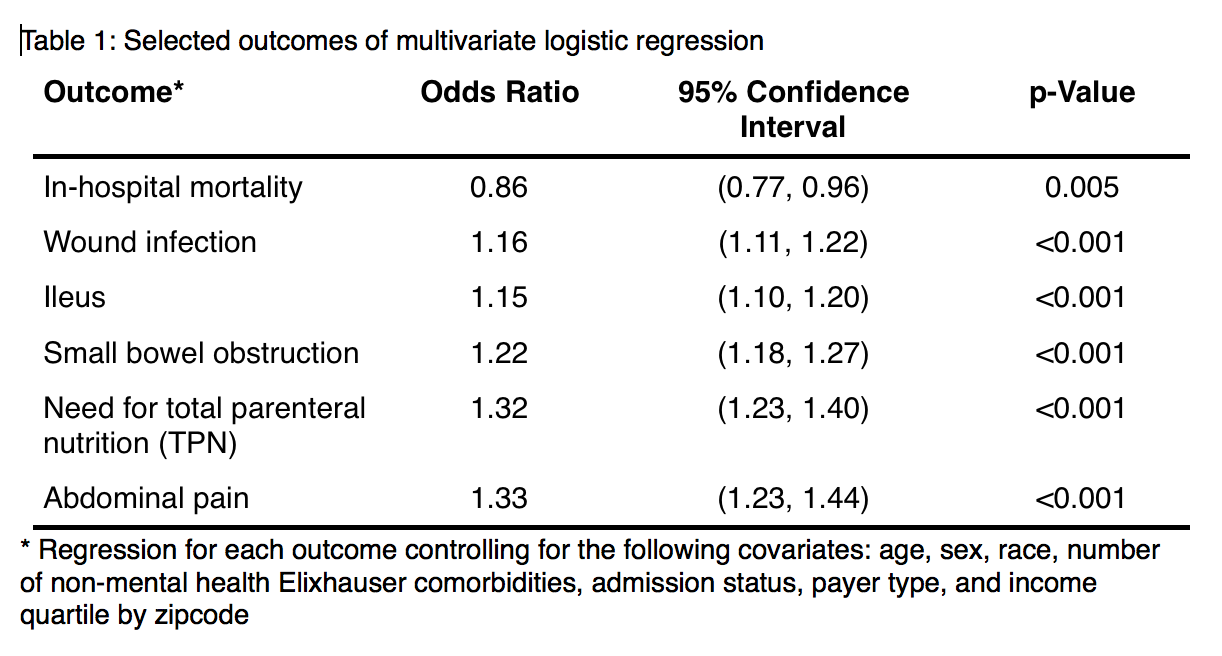
Results: 579,851 patients were included. 38,702 patients (6.67%) had a concurrent mental health diagnosis on admission. Of these, mood disorders were most prevalent at 58.7% (n=22,717) followed by substance abuse (23.8%, n=9,206), schizophrenia (13.5%, n=5,234), anxiety disorders (11.6%, n=4,484), and impulse control disorders (5.3%, n=2,059). Patients with mental health disorders were significantly younger than those without a mental health diagnosis (median 52 v 54 years; p<0.001). Those in the mental health cohort were significantly more likely to be female (61.1% v 57.6%), white (77.8% v 69.2%), and have a greater number of non-mental health comorbidites. They were also more likely to be admitted urgently or emergently (73.9% v 70.1%), insured by either Medicare or Medicaid (53.2% v 43.4%), and in the lowest income quartile by zipcode (27.8% v 24.9%). LOS for patients with co-morbid mental illness was 0.8 days longer (p <0.001). Co-morbid mental illness was significantly associated with any post-operative complication and specifically wound infection, ileus, small bowel obstruction, need for parenteral nutrition, and abdominal pain (Table 1). Odds of death were slightly lower in the mental health diagnosis cohort.
Conclusion: Patients who undergo the most common general surgery procedures with co-morbid mental health conditions experience a greater incidence of post-operative complications and longer hospitalizations. Recognizing disparate outcomes is the first step in understanding how to optimize care for this often marginalized population.