S. A. Christie1, D. C. Dickson1, T. Nana1, P. M. Stern1, A. Mbiarikai1, R. A. Dicker2, A. Chichom-Mefire3, C. Juillard1 1University Of California – San Francisco,Center For Global Surgical Studies,San Francisco, CA, USA 2University Of California – Los Angeles,Los Angeles, CA, USA 3University Of Buea,Department Of Surgery And Obstetrics- Gynecology, Faculty Of Health Sciences,Buea, SOUTHWEST REGION, Cameroon
Introduction:
Road traffic injury (RTI) is believed to be a major contributor to death and disability in sub-Saharan Africa. Existing data are predominantly derived from hospital or police records, leading to underreporting in areas where many people do not access formal care. To fill this epidemiologic gap and inform prevention policy, we conducted a community-based survey to identify the yearly incidence, patterns, and impact of road traffic injury in Southwest Cameroon.
Methods:
Three-stage cluster sampling with selection probability proportionate to population was used to select 36 enumeration areas in Southwest Cameroon. Household representatives at each site were asked to report all injuries in the preceding 12 months that resulted in death, loss of routine activity, or required medical attention. Data on injury mechanism, care-seeking behavior, cost of treatment, disability and economic impact were collected.
Results:
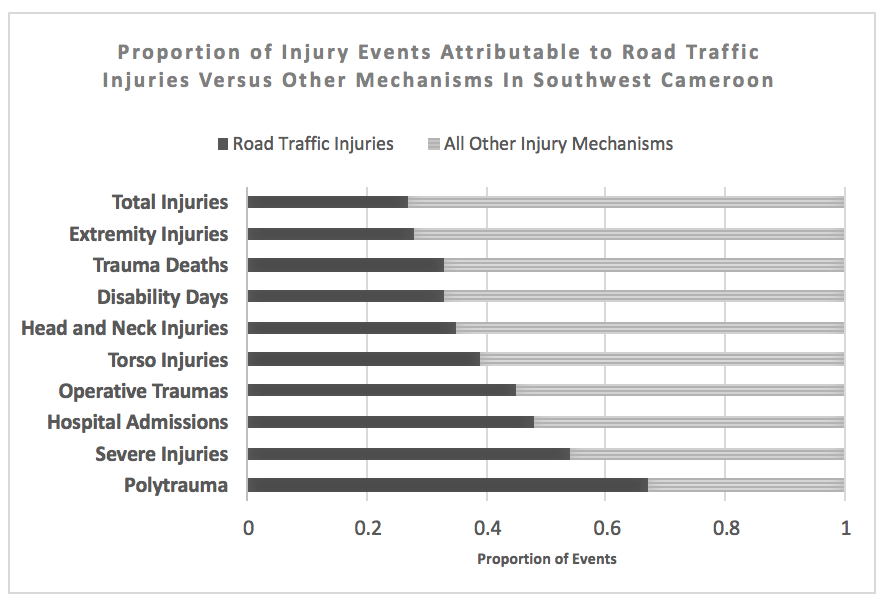
Road traffic injury was the largest single-mechanism contributor to trauma-related death and disability. [Figure] Among 8065 individuals in 15 rural and 18 urban areas, 133 RTI were identified for a total incidence of 16.5 RTI /1000 person-years (95CI 14-20). Incidence of fatal RTI was 37/100,000 person-years (95CI 13-105). Although RTI rates were higher in urban areas (18 vs 11/1000 person-years), incidence of RTI death was higher in rural or semirural regions (60 vs 20/100,000 person-years). Commercial transport vehicles were involved in 78% of RTI but few commercial drivers participated in first-aid or victim transport (7.5%). Seatbelts and helmets were very rarely utilized (7.6% and 8.7% respectively). Signs of severe injury including loss of consciousness, confusion, amnesia, or respiratory arrest at the scene occured in 34% of RTI. Formal medical services were sought for 79% of road traffic injuries; among those, 45% were admitted to inpatient care and 8.9% underwent at least one operation. Overall, RTI led to 480 disability days/1000 person-years with 24% of injuries resulting in ongoing disability at the time of the survey. Cost of RTI care was more than double the cost for non-RTI injury mechanisms (64,000 vs. 28,000 CFA, p<0.001) and 46% of RTI resulted in the affected household being unable to afford basic necessities.
Conclusion:
RTI occurs commonly in Southwest Cameroon and results in considerable physical and economic disability. As road safety prevention measures are rarely employed, policy modifications including increased monitoring of seatbelt and helmet compliance and offering first-aid training for commercial vehicle operators represent areas of potential opportunity to reduce disability and injury mortality in Cameroon.