L. Fluke1, R. Restrepo1, B. Hoagland1, J. Stephenson1 1Naval Medical Center Portsmouth,General Surgery,Portsmouth, VIRGINIA, USA
Introduction:
Full thickness soft tissue defects from congenital absence or traumatic loss are difficult to surgically manage. Healing requires cell migration, organization of an extracellular matrix (ECM), inflammation, and wound coverage.
We have previously shown that Poly(L-lactide) (PLLA) nanofibrous scaffolds enhance cell infiltration in vitro and in vivo in wound healing models, and we have demonstrated that the PLLA scaffold provides adequate strength to serve as a replacement for a full thickness abdominal wall defect in the rat model. Our current study compares aligned and unaligned nanofibrous scaffolds to a commonly used absorbable mesh, Vicryl, and permanent mesh, Gortex. We hypothesized that aligned electrospun PLLA nanofibrous grafts best facilitate native tissue ingrowth, providing physiologic strength necessary for repair of soft tissue defect while serving as a scaffold to guide tissue regeneration.
Methods:
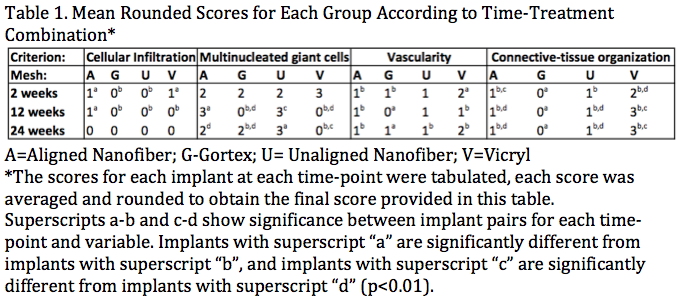
Abdominal wall defects were created in 72 rats, 6 rats per mesh per time frame, followed by underlay implantation of Vicryl, Gortex, aligned or unaligned PLLA Nanofiber mesh. Abdominal walls were harvested at 2, 12, and 24 weeks. Histopathologic semiquantative analysis was graded for cellular infiltration, multinucleated giant cells (MNG), vascularity, and tissue organization in a blinded fashion by an expert reviewer using a validated scoring system. Mean scores were compared and analyzed with non-parametric Mann-Whitney Wilcoxon testing.
Results:
Both aligned PLLA and Vicryl showed improved cellular infiltration at 2 weeks versus unaligned PLLA and Goretex. At 12 weeks, only the aligned PLLA had persistent cellular infiltration of the graft, while both aligned and unaligned PLLA grafts showed the presence of multinucleated giant cells (MNG). The presence of MNG’s decreases in the aligned PLLA graft by 24 weeks. There was no significant difference in graft vascularity at any timepoints. Vicryl graft had significant disruption at 2 and 12 weeks resulting in moderately organized connective tissue by the end of the study. Meanwhile, both aligned and unaligned PLLA grafts were broken down with less densely organized connective tissue, or scar.
Conclusion:
PLLA graft maintains structural integrity until at least 12 weeks and exhibits substantial tissue replacement at 24 weeks. Vicryl and PLLA grafts have similar tissue responses; however the Vicryl mesh has substantial degradation at 2 weeks and results in more dense scarring. These results demonstrate that PLLA Nanofiber mesh offers early strength comparable to Gortex but breaks down, replaced with cellular growth creating a favorable option in management of complex surgical wounds or native soft tissue defects.