S. N. Acker1, B. Bredbeck1, D. A. Partrick1, A. M. Kulungowski1,2, C. C. Barnett2, D. D. Bensard1,2 1Children’s Hospital Colorado,Pediatric Surgery,Aurora, CO, USA 2Denver Health Medical Center,Department Of Surgery,Denver, CO, USA
Introduction: The 6 criteria for highest trauma team activation include systolic blood pressure (SBP)< 90mmHg for adults or age-adjusted hypotension for children. These criteria aim to identify injured patients who likely require emergent intervention requiring trauma team presence. We have previously demonstrated that shock index, pediatric age adjusted (SIPA) accurately identifies severely injured children following blunt trauma. We hypothesized that elevated SIPA would more accurately identify injured children requiring highest trauma team activation and emergent intervention than age adjusted hypotension.
Methods: We performed a retrospective review of all children age 4-16 admitted to one of two trauma centers following blunt trauma with an injury severity score >15 from 1/07- 6/13. Indicators of need for trauma team activation included blood transfusion, emergent operation (including craniotomy, intracranial pressure monitor or drain, chest tube, thoracotomy, aniogembolization, or laparotomy), or endotracheal intubation (ETI) within 24 hours of admission. SIPA represents the maximum normal shock index (SI) for a given age group and was derived based on the maximum normal HR divided by the minimum normal SBP for each age group. Cutoffs included SI >1.22 (age 4-6), >1.0 (7-12), and >0.9 (13-16). Age adjusted hypotension cutoffs were as follows: SBP <90 (age 4-6), SBP <100 (7-16).
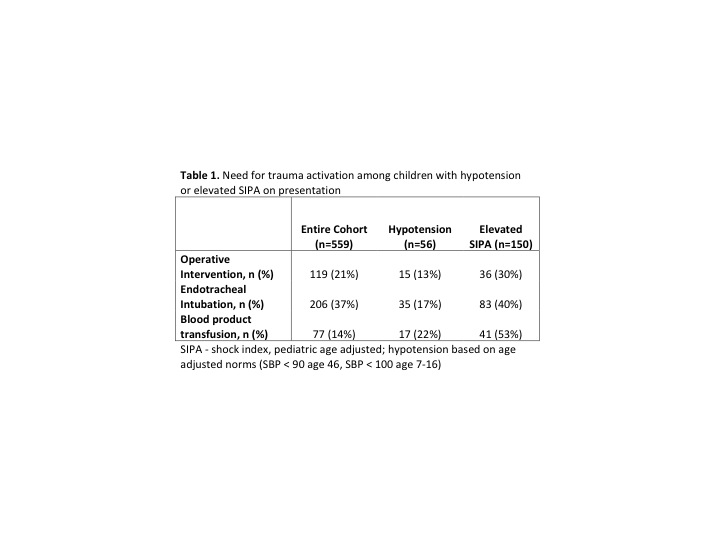
Results:559 children were included; 21% underwent operation, 37% ETI, and 14% blood transfusion within 24 hours of admission. 56/559 (10%) were hypotensive. 150/559 (27%) had an elevated SIPA. Hypotension alone poorly predicted the need for operation (13%), ETI (17%), or blood transfusion (22%). In contrast, operation (30%), ETI (40%), and blood transfusion (53%) were more likely in children with an elevated SIPA (Table 1). 25 children required all three interventions, 3 (12%) were hypotensive at presentation, 15 (60%) had an elevated SIPA (P<0.001).
Conclusion:
Elevated SIPA is superior to age-adjusted hypotension to identify injured children likely to require emergent operation, ETI or early blood transfusion. 10% of injured children requiring early intervention demonstrated age specific hypotension. Using SIPA, an age-adjusted tool employing both heart rate and SBP, tripled the number of high-risk children identified who needed intervention. Still nearly half of significantly injured children requiring at least one acute intervention were not identified by either hypotension or SIPA. Thus, SIPA, like age-adjusted hypotension cannot be relied upon solely for trauma team activation. However, SIPA, rather than age-adjusted hypotension, should be considered as one of the six minimum criteria for trauma team activation.