A. Shakoor4, A. Shah2, C. K. Zogg1, A. H. Haider1, R. Riviello3, A. Latif6, F. G. Qureshi7, T. Oyetunji8, A. Mateen5, H. Zafar5 8Children’s Mercy Hospital And Clinics,Department Of Surgery,Kansas City, MO, USA 1Brigham And Women’s Hospital,Center For Surgery And Public Health, Harvard Medical School, Harvard T H Chan School Of Public Health,BOSTON, MA, USA 2Mayo Clinic In Arizona,Department Of Surgery,Phoenix, AZ, USA 3Brigham And Women’s Hospital,Division Of Trauma, Burns And Surgical Critical Care,Boston, MA, USA 4West Virginia University School Of Medicine,Department Of Pediatrics, Charleston Area Medical Center (CAMC),Charlston, WV, USA 5Aga Khan University Medical College,Department Of Surgery,Karachi, Sindh, Pakistan 6Johns Hopkins University School Of Medicine,Department Of Anesthesia,Baltimore, MD, USA 7Children’s National Medical Center,Department Of Surgery,Washington, DC, USA
Introduction:
Whether adult general surgeons, in addition to pediatric specialists, should handle pediatric emergency general surgery (EGS) remains controversial. Unlike surgical centers in higher income countries, resource-limited settings in low-middle income countries often lack staff, resources, and training needed to maintain ready access to specialist care, making treatment by general surgeons an imperative. The objective of this study was to examine differences in surgical outcomes among children/adolescents managed by pediatric versus adult surgical teams for EGS conditions presenting to a regional tertiary hospital in South Asia with split patient coverage between pediatric and adult surgical teams.
Methods:
Pediatric patients (<18y) admitted to the Aga Khan University Hospital in Karachi, Pakistan, with an EGS diagnosis (defined by the AAST) between March 2009 and April 2014 were included. Patients were dichotomized into those managed by adult versus pediatric teams. Differences in length of stay (LOS), mortality, and major complications were compared between the two groups using descriptive statistics and multivariable linear (family gamma; link log)/logistic regression. Propensity scores accounted for potential confounding associated with demographic/clinical factors.. Quasi-experimental counterfactual models examined hypothetical differences in outcomes, assuming that all patients were managed by pediatric teams.
Results:
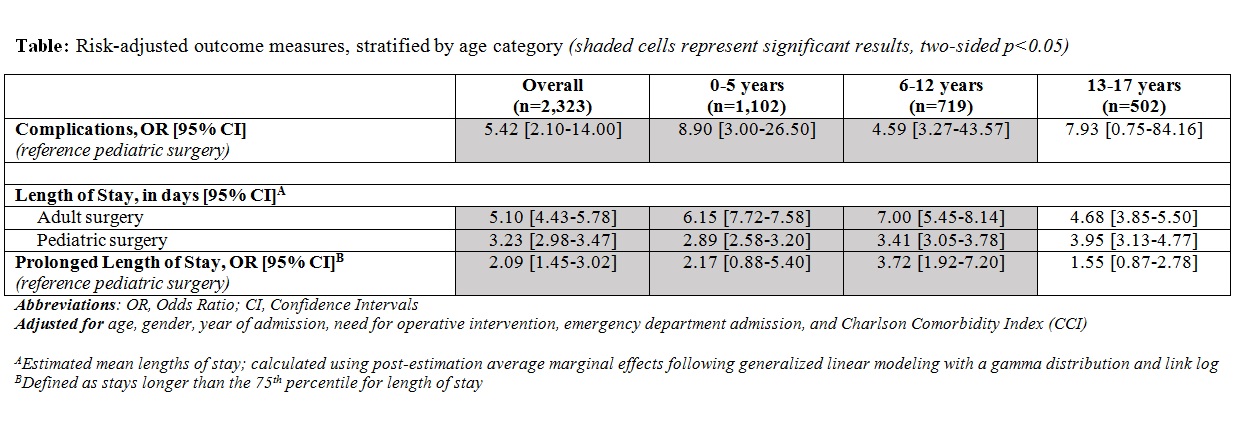
A total of 2,323 patients were included. Average age was 7.1y (±5.5 SD); most were male (77.7%). The majority, n=1,958, was managed by pediatric specialty teams; however, 365 patients received treatment from adult general surgery teams. 42 patients (1.8%) developed complications; 21 (0.9%) died (all adult general surgery). Relative to patients managed by pediatric surgery, patients managed by adult surgery had 5.42 times higher risk-adjusted odds of developing complications (OR[95%CI]: 5.42[2.10-14.00]) and longer average LOS (predicted mean difference: 1.87[1.45-2.31] days). Counterfactual models suggest that patients at Aga Khan would have experienced 39.8% fewer complications and a 36.7% relative reduction in average LOS if all patients had been managed by pediatric surgery.
Conclusion:
In light of recent work by the Lancet Commission and DCP3, it becomes important now, more than ever, to address questions related to relevant development efforts in both burgeoning and established global surgical fields. Beyond efforts to establish surgical capacity, the results of this study speak to a need for health systems strengthening, suggesting that, where possible in resource-constrained settings, efforts should be allocated to promote development/staffing of diverse surgical teams.