L. Xu1, Y. Kim1, F. Gani1, G. A. Margonis1, D. Wagner1, S. Buttner1, T. M. Pawlik1 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA
Introduction: Skeletal muscle depletion (SMD) has been shown to be a powerful predictor of a poor prognosis. We sought to identify the prevalence of sarcopenia and low muscle attenuation (MA) among patients undergoing hepato-pancreatico-biliary (HPB) surgery, as well as the prognostic value of SMD for HPB surgery.
Methods: Patients undergoing HPB surgery between August 2011 and June 2014 with available preoperative (≤30 days) lumbar computed tomography (CT) images were identified. Total psoas volume (TPV) and average psoas density (PD) were measured using preoperative CT scans. Sarcopenia was defined as the lowest gender-specific quartile for TPV. Similarly, low MA was defined as the lowest gender-specific quartile for PD. SMD was defined as presence of both sarcopenia and low MA. Patients with missing data for TPV, PD, or BMI, and patients <18 years were excluded from the analysis. Clinical features, complications, short-term outcomes and overall survival of patients were collected.
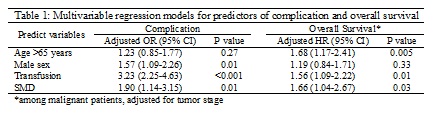
Results: Of the 913 patients included, the median age was 63 years (IQR 53, 71) with 47.3% being male. Over two-thirds (n=633, 69.3%) of patients underwent surgery for a malignant disease. Patients undergoing surgery for a malignant disease were older (median 64 years vs. 59 years, p<0.001), and more likely to be male (57.2% vs. 42.5%, p<0.001). Of note, BMI was not different between patients undergoing surgery for malignant or benign disease (p=0.682). Sarcopenia and low MA were more common in patients with malignant disease (sarcopenia 27.7% vs. 19.3% in benign, p=0.007; low MA 27.5% vs. 19.3%, p=0.008). Among the entire cohort, patients presenting with SMD reported a higher incidence of postoperative complications (31.6% vs. 15.8% in non-SMD patients, p<0.001), as well as longer length of stay (median 11 days [IQR 7, 16] vs. 8 days [IQR 6, 12] in non-SMD patients, p<0.001). Among the patients undergoing surgery for malignant disease, patients with SMD had a higher risk of death than patients without SMD (HR 1.8, 95% CI 1.1-2.9; p=0.01). On multivariate analysis, SMD was remained as an independent predictor for both complication (OR 1.90, 95% CI 1.14-3.15; p=0.01) and a worse overall survival (HR 1.66, 95% CI 1.04-2.67; p=0.03).
Conclusions: Sarcopenia and low MA are more common in patients undergoing HPB surgery for malignant disease compared to patients with benign disease. SMD is an independent predictor of poor prognosis in patients undergoing HPB surgery.