G. MARGONIS1, Y. Kim1, F. Gani1, T. M. Pawlik1 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA
Introduction: The influence of intraoperative blood loss (IBL) on long-term outcomes of patients undergoing liver resection for colorectal cancer liver metastases (CRLM) remains not well defined. We sought to study the prognostic impact of intraoperative blood loss on long-term survival following resection of CRLM.
Methods: A total of 433 patients who underwent hepatic resection with curative intent for CRLM between 2000 and 2013 at a major hepatobiliary center were identified. Demographics data, operative details, intraoperative blood loss data, and long-term outcomes were collected and analyzed. IBL cutoff volume was calculated using chi square test analysis. Clinicopathologic predictors of IBL were identified using logistic regression. Overall survival (OS) was assessed using the Kaplan-Meier and Cox regression methods.
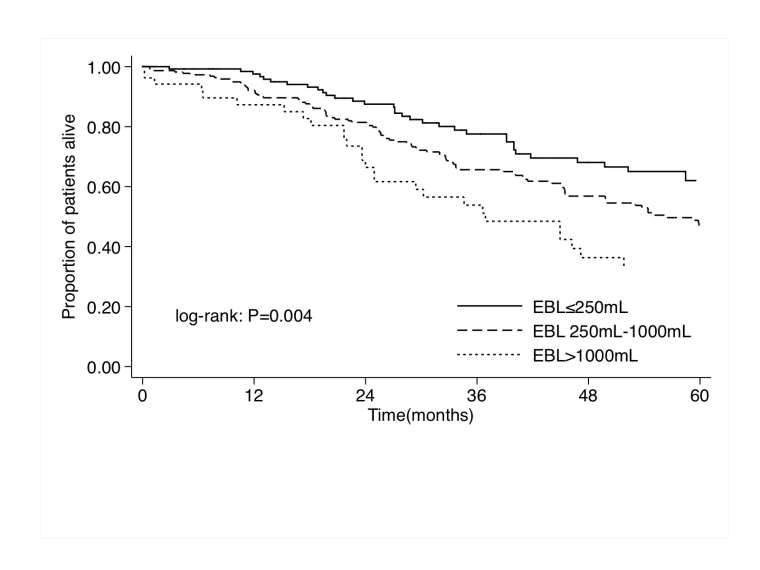
Results:Median patient age was 54 (IQR 44, 64) years, and the majority of patients were male (58.9%, n=255). At the time of surgery, the median IBL was 400 (IQR 200-800) mL. Intraoperatively, 146 (33.7%) patients had an IBL <250 mL, while 287 (66.3%) patients had an IBL ≥250 mL. On multivariate analysis, factors associated with IBL ≥250 mL included male sex (OR 2.62, 95%CI 1.69-4.08; P<0.001), tumor size >3cm (OR 1.88, 95%CI 1.18-2.99; P=0.01), and major hepatic resection (OR 3.07, 95%CI 1.93-4.90; P<0.001). At a median follow-up time of 30.6 months, median and overall 5-year survival were 59.9 months and 49.3%, respectively. Of note, IBL was associated with both median and 5-year survival (<250 mL: 70.5 months, 62.0% vs. 251-1000 mL: 56.4 months, 46.1% vs. >1000 mL: 36.9 month, 33.0%, respectively; P=0.004, Figure). On multivariable analysis, tumor specific factors such as primary tumor N stage (HR 1.42, 95%CI 1.04-1.95; P=0.03) and tumor size >3 cm (HR 1.48, 95%CI 1.11-1.98; P=0.01), as well as procedure factors such as use of ablation (HR 2.31, 95%CI 1.59-3.34; P<0.001) were associated with overall survival. Of note, IBL also remained an independent prognostic factor of long-term survival even after controlling for whether the patient did or did not receive a blood transfusion (HR 1.48, 95%CI 1.06-2.07; P=0.02).
Conclusion:The magnitude of IBL during CRLM resection was related to biologic characteristics of the tumor as well as the extent of surgery. Increased IBL during CRLM resection was an independent prognostic factor associated with a worse long-term survival.