A. Albaghdadi1, J. Canner1, E. B. Schneider1, C. B. Feather1, J. Odden1, E. R. Haut1 1Johns Hopkins University School Of Medicine,Baltimore, MD, USA
Introduction:
Controversy remains about the ideal approach for cervical spine clearance in obtunded, blunt, adult trauma patients. An EAST practice management guideline was recently published suggesting that MRI is not necessary in hopes of standardizing care. We aimed to identify national variation of MRI use to clear the c-spine in obtunded trauma patients and describe patient- and hospital-level factors associated with its use.
Methods:
We conducted a retrospective review of the NTDB from 2007 to 2012. We included blunt trauma patients >=18 years, treated at level 1 or 2 trauma centers (TCs), with a GCS<=8, Head AIS>3 and mechanically ventilated >72 hours. The proportion of patients undergoing MRI at each hospital was calculated. Multi-level modeling was used to identify patient- and hospital- level factors associated with MRI use.
Results:
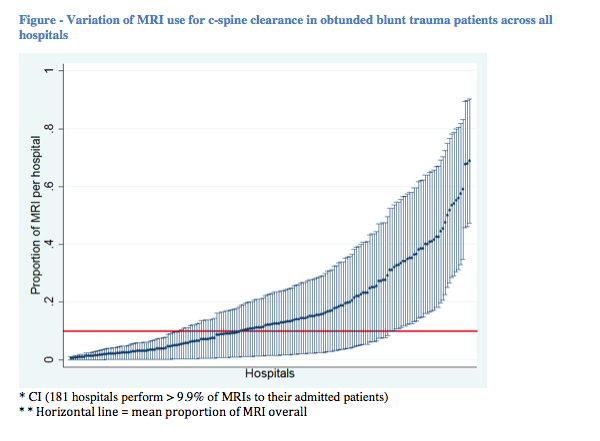
We included 32,125 patients treated at 395 unique TCs. The mean proportion of MRI over the entire sample was 9.9%. Amongst the 181 hospitals (57.8% of all admissions) that performed and reported MRIs, the proportions of patients who received MRI per hospital ranged from 0.5-68.4%. (Figure) Younger patients, MVC and pedestrian injuries were more likely to receive an MRI. Injury severity (ISS) was not associated with MRI use. Hospitals in the northeast, level 1 TCs, and non-teaching hospitals were more likely to perform MRI.
Conclusion:
After controlling for patient-level characteristics, variation remained in MRI use based on hospital specific, geographic, trauma center level, and teaching status characteristics. Cervical spine clearance protocol implementation based on the new EAST guideline may standardize care, reduce variation in practices, and decrease healthcare costs.