W. A. Young1, E. A. Fallon1, C. P. Erickson1, C. S. Muratore1, W. G. Cioffi1, D. S. Heffernan1, A. Ayala1 1Brown University School Of Medicine,Division Of Surgical Research,Providence, RI, USA
Introduction:
Sepsis and specifically neonatal sepsis, remains a major contributor to morbidity and mortality. Modeling neonatal sepsis remains a challenge. A recently described murine model of cecal slurry has offered exciting promise in mimicking neonatal sepsis. Further, with respect to sepsis induced immune pathways alterations, our laboratory has noted a key role for a family of co-inhibitory molecules in adult septic mice and ICU patients, which may be a target for development of novel therapies. We examine the role of one co-inhibitory molecule, programmed death receptor-1 (PD-1) in an evolving model of neonatal sepsis.
Methods:
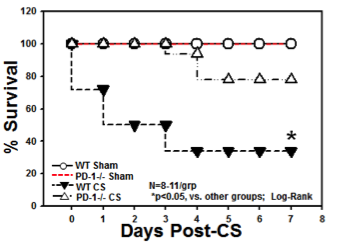
Our cecal slurry model consists of harvesting the cecal contents of an adult wild type (Wt) mouse and combining it with 5% dextrose to create a slurry with a concentration of 80mg/ml (LD70 at 7 days). Neonatal mice (5-7 days of age) from both C57BL/6 Wild type and PD-1 knockout underwent intraperitoneal injection (IP) of the cecal slurry (CS) versus IP of 0.9% saline for sham procedure (Sh). Western blot and immunohistochemistry were performed to assess for differential expression of PD-1. Cytometric bead array was utilized to identify changes in circulating cytokine expression. H&E was used for tissue morphology of liver, lung and cardiac tissue. Survival studies following CS and Sh in Wt and PD-1 knockout were performed and analyzed by the Kaplan-Meier method.
Results:
Presence of intra-abdominal sepsis was confirmed by bacterial count of peritoneal lavage (PL) at 24 hours. PL of CS mice had 7.89 x 105 CFU/microliter vs 0 CFU/microliter in the Sh pups (p<0.05). Histologic assessment of organ specimens demonstrated alterations in tissue architecture and cell response most notable in lung, liver and thymus. Liver and thymus specimens of Wt CS mice showed apoptosis that was not present in the Wt Sh group. However, PD-1 knockout mice undergoing CS demonstrated decreased apoptosis compared to Wt. Septal thickening was present in lung specimen of Wt CS pups, which was again attenuated in CS PD-1 knockout mice. Wt CS mice had significantly decreased survival when compared to Sh, however, PD-1 mice undergoing CS had improved survival when compared to their Wt counterparts.
Conclusion:
We demonstrate with a novel model of neonatal sepsis, that the checkpoint protein, PD-1, plays an important role in the development in morbidity and mortality following sepsis. Given that these molecules are altered in the neonatal and adult murine models of sepsis and are elevated in critically ill septic patients, this implies that PD-1 may be a promising potential target for improving outcomes in sepsis.