B. Parent1, B. Hamilton2, B. Henley2, G. O’Keefe1, J. Agel2, A. Garman3, R. Firoozabadi2 1University Of Washington,General Surgery,Seattle, WA, USA 2University Of Washington,Orthopedic Surgery,Seattle, WA, USA 3University Of Washington,Nutrition,Seattle, WA, USA
Introduction:
Malnutrition is associated with poor outcomes in surgical patients, including wound infections, longer length of stay, and increased mortality. Targeted nutrition interventions have well-established benefits in critical-care and general surgery trauma populations, but have not been studied in a large cohort of orthopedic trauma patients. The aim of this study was to evaluate a targeted daily nutrition intervention in this population, and to measure its impact on biochemical indices of nutrition and clinical outcomes.
Methods:
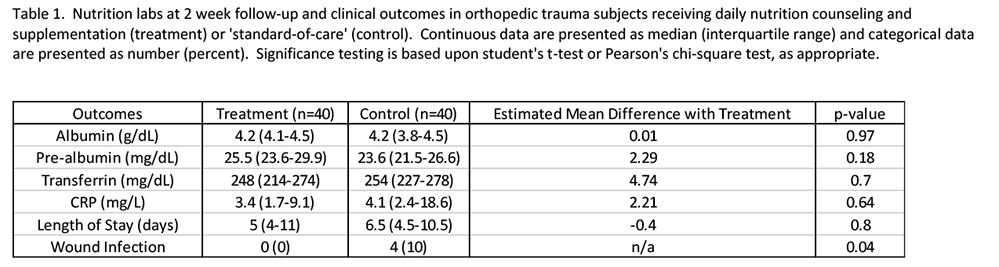
Adult patients (age 18-65 years-old) admitted to the orthopedic surgery service with extremity fractures were included in this trial. Patients were excluded if they had multi-system injury which required admission to another surgical service. Upon admission, subjects were randomized to receive either: a) daily nutrition counseling from a dietitian with supplementation of antioxidants, micronutrients, and protein or b) standard-of-care. Serum levels of albumin, pre-albumin, C-reactive protein, and transferrin were obtained on days 1,3,7 and at 2 weeks. The number of missed meals, daily protein and calorie intake, length of hospital stay, and the incidence of wound infections were also recorded. A student’s t-test, Pearson’s chi-square test, and multiple linear regression were used to ascertain statistical significance.
Results:
80 subjects were enrolled (40 in each arm). The cohort was 46% female, with a median age of 47. 72% had fractures of the femur, tibia or ankle, and 15% had fractures of the humerus or forearm. Over the first week, intervention and control arms showed no differences in the median number of missed meals [6 (3.5-8) versus 4.5 (2.5-8.5), p=0.31], grams of protein intake [240 (165-401) versus 289 (149-378), p=0.91], or calorie intake [6035 (4592-9081) versus 7234 (4321-9832), p=0.64]. Intervention and control arms did not differ in any of the measured biochemical indices of nutrition (Table 1). A subgroup analysis comparing patients in the upper quartile of calorie and protein intake to those in the lower quartile also revealed no differences in nutrition labs. There were fewer wound infections (0 versus 4, p=0.04) in the intervention arm.
Conclusion:
During the first week of admission, daily nutrition counseling does not appear to impact calorie, protein or meal intake in orthopedic trauma patients. Moreover, traditional biochemical indices for nutrition status do not correlate well with levels of intake. These data may indicate that current metrics for evaluation of nutrition status and intake are not clinically relevant in this population. This highlights a need for alternative diagnostic tools and novel therapeutic targets in nutrition science.