A. Ranjit1, W. Jiang1, M. A. Chaudhary1, T. Zhan1, E. B. Schneider1, S. L. Cohen2, A. H. Haider1, S. E. Little2, J. N. Robinson2 1Brigham And Women’s Hospital,Center For Surgery And Public Health,Boston, MA, USA 2Brigham And Women’s Hospital,Obstetrics And Gynecology,Boston, MA, USA
Introduction: Ectopic pregnancy (EP) is the leading cause of first trimester pregnancy-related death. Laparoscopic surgery (LS) for EP is associated with shorter length of stay and operation time along with less intra-operative bleeding. Racial disparities in laparoscopic surgery (LS) for ectopic pregnancy (EP) are documented and are generally attributed to unequal access to care. The objective of this study was to determine if racial disparities exist in the receipt of LS for EP among universally insured population.
Methods: Using 2006-2010 TRICARE (universal insurance coverage to all members of US Armed Services and their dependents) claims data, tubal EP patients who received surgical intervention (LS or laparotomy) for EP within 48 hours and 30 days of diagnosis were identified using ICD-9 and CPT codes. Cases were then stratified into direct (military hospital) or purchased (civilian hospital) systems of care. Patient demographic characteristics were compared between each racial group (White, Black and Asian/Pacific Islander). Unadjusted and adjusted odds of receipt of LS in each racial group for surgeries performed within 48 hours and 30 days of diagnosis were compared adjusting for patient demographics, system of care and severity of EP. Sub-analysis for odds of receipt of LS for each racial group within direct and purchased care systems was performed.
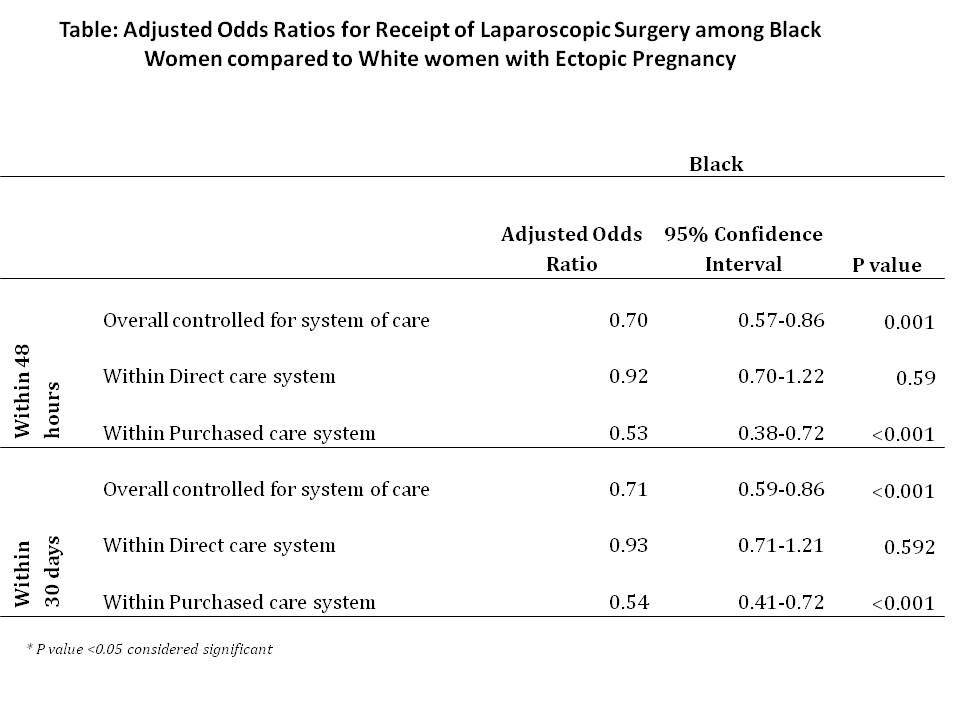
Results:Among a total of 2680 tubal EP who received surgical intervention, 1620 (60.4%) received LS and 1060 (39.5%) received laparotomy for EP within 30 days of diagnosis. Ninety-one percent of these surgeries were performed within 48 hours of initial diagnosis and 52% were performed within purchased care system. Among all cases identified, 1692 (63.13%) were White, 169 (6.31%) Asian and 819 (30.56%) Black. Overall, 40.9% of White women received LS compared to 32.1% Asian and 33.7% Blacks (p-value: <0.001) within 48 hours. On multivariable analysis adjusted for demographic factors, system of care and severity of EP, Blacks were 30% less likely to receive LS for EP within 48 hours of initial diagnosis. These disparities were not present within the direct system of care (OR: 0.92; CI: 0.70-1.22) but were only present within the purchased system of care (OR: 0.53, CI: 0.38-0.72). Similar trends were seen for surgeries performed within 30 days of initial diagnosis. [See Table]
Conclusion:Black women were less likely to receive LS for EP within purchased care (civilian hospital) in the universally insured TRICARE population. These findings might help inform policy changes to ensure equal access to advanced surgical options among all beneficiaries irrespective of race and system of care.