F. Gani1, M. Daniel1, J. Hundt1, J. E. Efron1, M. A. Makary1, T. M. Pawlik1 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA
Introduction: Reducing unwanted variations in healthcare has been identified as an opportunity for cost containment. We sought to characterize variations in hospital costs for several surgical procedures and quantitate the variability attributable to the patient, procedure, and provider.
Methods: Patients who underwent coronary artery bypass grafting (CABG), open abdominal aortic aneurysm repair (AAA), laparoscopic cholecystectomy (LC), pancreatectomy or colectomy between 2009 and 2013 were identified at a large tertiary care hospital. Inter- and intra-provider variations in costs were compared using coefficient-of-variation (CV). Multivariable hierarchical linear modeling was utilized to quantitate variation in total hospital costs attributable to the patient, procedure and provider.
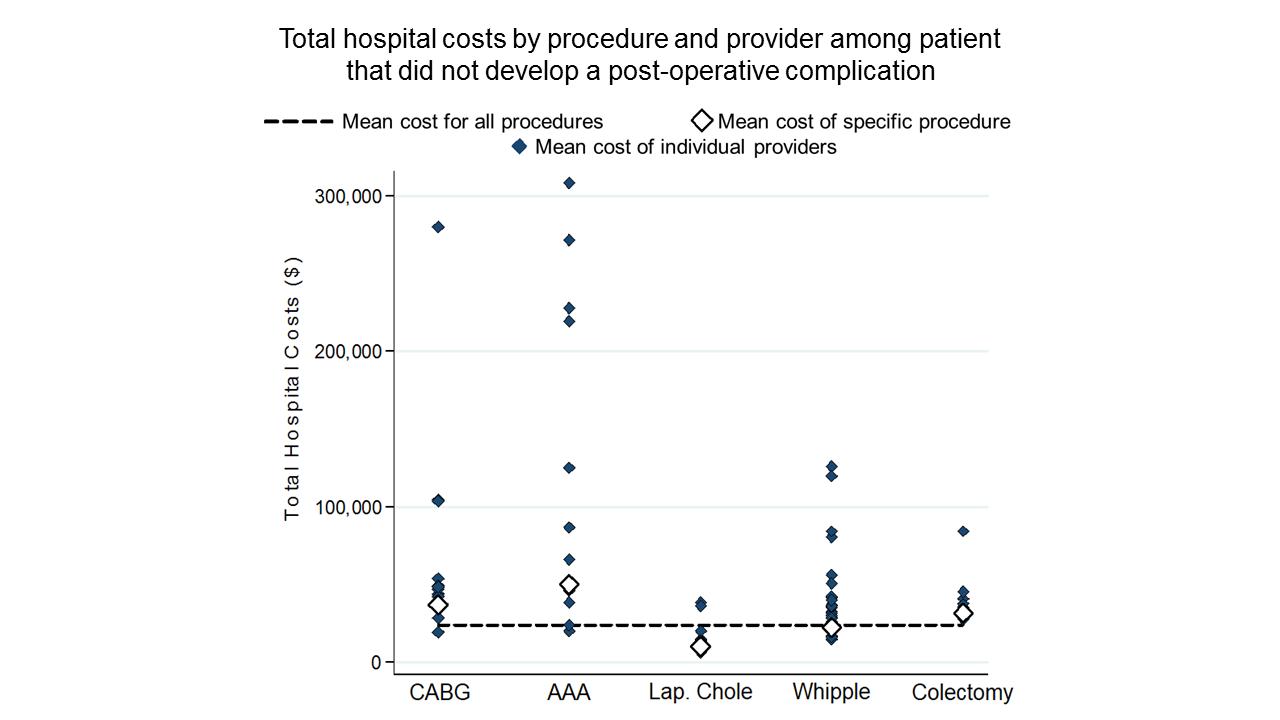
Results: Among the 4,802 patients that underwent surgery, the average cost of surgery was $34,697 (SD=25,844) ranging from $11,177 (SD=$4,955) for LC to $63,654 (SD=54,046) for AAA repair. While perioperative complications resulted in increased cost (no complication: $25,864, SD=16,838 vs. complication: $47,171, SD=72,692, p<0.001), total hospital costs remained variable even among patients without complications (p<0.001, Figure). Substantial variation in total costs was observed among surgeons performing the same surgery (CV: CABG, 103%; AAA, 104%, LC, 69%, pancreatectomy, 82%; colectomy, 122%). Further, marked variations in costs were also observed within the same surgeon performing the same surgery (CV: CABG, 21%-116%; AAA, 26%-111%, LC, 19%-107%, pancreatectomy, 31%-101%; colectomy, 17%-155%). After accounting for patient comorbidity, postoperative complications and length of stay, 90% of total variability was explained by patient- and procedure-related factors, while 10% was attributed to variations in surgeon practices.
Conclusion: Hospital procedure costs varied markedly among and even within providers. While patient level factors explained most of the variation in cost, up to 10% of the variation was due to provider-level differences, which can be a potential target for cost containment.