D. S. Swords1, M. A. Firpo1, K. M. Johnson1, K. M. Boucher2, C. L. Scaife1, S. J. Mulvihill1 1University Of Utah,General Surgery,Salt Lake City, UT, USA 2University Of Utah,Study Design And Biostatistics Center,Salt Lake City, UT, USA
Introduction: The TMN staging system of the American Joint Commission on Cancer (AJCC) is designed to stratify patients by anatomic extent of disease. It is expected that patients with progressively advanced stages will experience shorter survival. We examined how well the AJCC staging system predicted survival for patients with pancreatic adenocarcinoma (PDAC) in the Surveillance, Epidemiology and End Results (SEER) research database. In an attempt to account for discrepancies in survival in intermediate stages in SEER data we also investigated the accuracy of clinical nodal staging in resected patients from our institution.
Methods: Data were abstracted from SEER Database from 2004-2012 and filtered for PDAC with known stage. The relation between stage and disease-specific survival was evaluated using Kaplan-Meier and Cox proportional hazard analyses. We also evaluated 110 consecutive cases at our facility from 2001-2014 that proceeded to resection without neoadjuvant therapy, comparing differences in clinical and pathological staging.
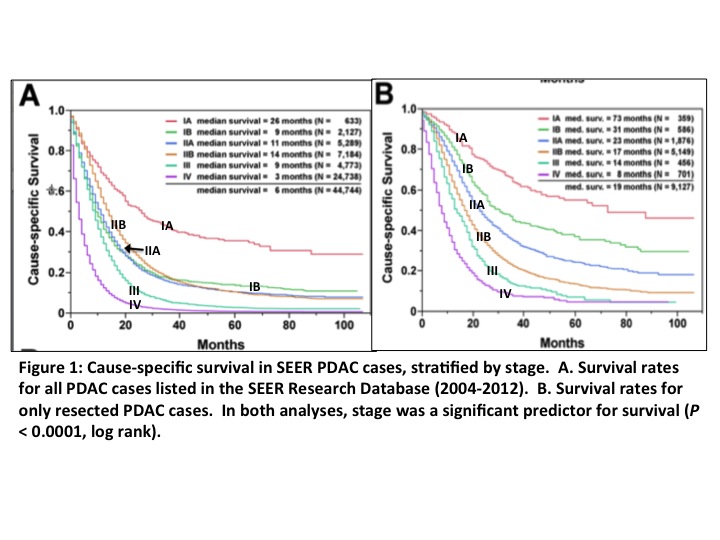
Results: 44,744 SEER cases met inclusion criteria. Median age was 67 and 51.7% were male. Tumor location was 52% in the head of the pancreas, 12% in the body, and 13% in the tail. Overall, resection was recommended in 25% and performed in 21%. In Stages IB and IIA resection was recommended in 39% and performed in 34% whereas in Stage IIB it was recommended in 73% and performed in 72%. Intermediate stages did not correlate well with the expected inverse relationship between stage and survival. We found longer survival for stage IIB than for stage IB (p<0.0001, log-rank test) and stage IIA (p<0.0001, log-rank test). However, in resected cases with pathological staging the expected inverse relationship between survival and extent of disease was evident (Figure 1). In 110 resected PDAC cases from our institution without neoadjuvant therapy, 89/110 (81%) were classified as N0 by clinical staging, whereas only 33/110 (30%) were N0 by pathological staging (p < 0.0001, Chi Square test). Only 40/110 (36%) were correctly classified for nodal status by clinical staging, with 26/110 (24%) correctly identified as N0 and 14/110 (13%) as N1. In the incorrectly classified cases, 63/70 (90%) were up-staged from N0 to N1 by pathological staging.
Conclusion: In evaluating AJCC staging of PDAC patients, survival between Stages IB, IIA, and IIB is paradoxical to what would be expected. This is likely due to clinical underestimation of nodal involvement. The high rates of surgical recommendation and resection in Stage IIB patients may reflect stage migration of patients due to unexpected nodal involvement. These findings have implications for treatment decisions in patients with intermediate stage PDAC.