A. A. Shah1,2, C. K. Zogg1, M. A. Chaudhary1, W. Jiang1, A. B. Chapital2, D. J. Johnson2, A. Ashraq2, A. Salim3, J. M. Havens3, Z. Cooper1, S. Nitzschke3, A. H. Haider1 1Brigham And Women’s Hospital,Center For Surgery And Public Health, Harvard Medical School, Harvard T H Chan School Of Public Health,Boston, MA, USA 2Mayo Clinic In Arizona,Department Of Surgery,Phoenix, AZ, USA 3Brigham And Women’s Hospital,Division Of Trauma, Burns And Surgical Critical Care,Boston, MA, USA
Introduction: Multiple measures of comorbidities have emerged for risk stratification of surgical patients. The Charlson Comorbidity Index (CCI) and the Elixhauser Comorbidity Index (ECI), are among the most commonly used in surgical outcomes research. While extensively studied in other areas of elective surgical care, limited assessment of their utility has been conducted for acute care surgery, beyond research in burns and extremity fractures. To that end, the objective of this study was to determine the relative predictive value of CCI vs ECI as comorbidity assessments in models of mortality and major complications for various subsets of acute care surgical patients.
Methods: Five years of data from the Nationwide Inpatient Sample (2007-2011) was queried for adult patients (≥18y) with a primary diagnosis of traumatic injury, emergency general surgery (EGS) — defined by the AAST – (critical subsets of acute care surgery) or emergent admissions for abdominal aortic aneurysm (AAA) repair, coronary artery bypass graft (CABG), and colectomy (major procedures associated with prevalent morbidity/morality). Base multivariable assessment models adjusted for a commonly utilized set of patient- and hospital-related factors, without consideration of comorbidities. Elaboration models considered both CCI and ECI as summary measures as well as by inclusion of individually identified comorbidities. Model discrimination was assessed using concordance (c) statistics.
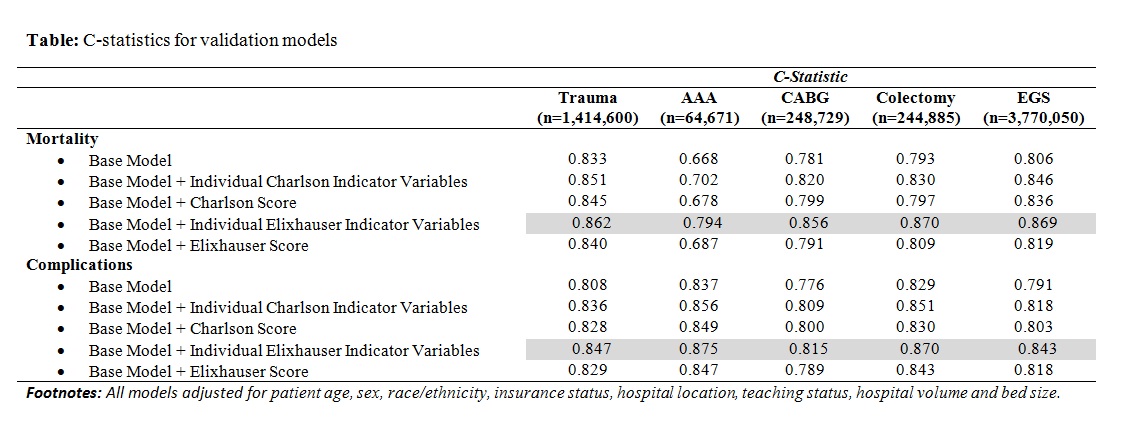
Results:A total of 5,742,935 patient records for acute care surgery were analyzed. Of these, 65.6% had an EGS conditions, 24.6% traumatic injuries, 4.3% underwent emergent CABG repair, 4.3% underwent emergent colectomy, and 1.2% underwent emergent AAA repair. Models comprising of the individual indicators of comorbidities for both Charlson and Elixhauser performed better than the weighted scores for both complications and mortality, for each diagnostic subgroup (Table). Addition of individual Elixhauser indicators of comorbidities considerably improved the discriminative ability of the model at predicting mortality (increase by 1.29% for trauma, 13.10% for AAA, 4.39% for CABG, 4.82% for colectomies & 2.72% for EGS) and complications (increase by 1.31% for trauma, 2.2% for AAA, 0.74% for CABG, 2.23% for colectomies & 3.05% for EGS) compared to the Charlson indicators of comorbidities (p<0.05).
Conclusion:Elixhauser and Charlson’s comorbidity indices both displayed good discrimination ability. However individual Elixhauser comorbidity measures performed the best in both morbidity and mortality models. This bares implications on the use of Elixhauser indicators of comorbidity for risk stratification of acute care surgery patients in administrative datasets.