K. Law2, A. N. Rutherford3, S. J. Gannon1,4, C. T. Millar1, C. M. Pugh1,2 1University Of Wisconsin,Department Of Surgery,Madison, WI, USA 2University Of Wisconsin,Department Of Industrial And Systems Engineering,Madison, WI, USA 3University Of Wisconsin,Health Professions,La Crosse, WI, USA 4University Of Wisconsin,Kinesiology,Madison, WI, USA
Introduction: Surgery requires the effective coordination of both dominant and non-dominant hands; however, switching attention between hands during operative tasks can increase cognitive load, leading to longer movement planning and execution times. Researchers have previously investigated the impact of hand dominance on performance and dexterity using focused, psychomotor tasks; however, few efforts have attempted to understand the importance of these skills at the procedural level. The study aim was to identify residents’ coordination between their dominant and non-dominant hands while they grasp for sutures during a simulated laparoscopic ventral hernia repair.
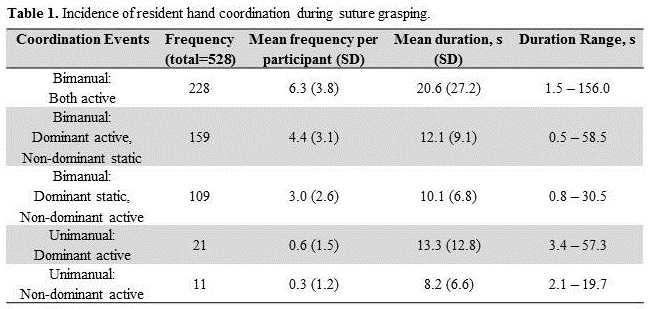
Methods: Residents (PGY2-4) had 15 minutes to complete two steps of a simulated laparoscopic ventral hernia procedure. Residents self-reported their hand dominance in a pre-simulation survey. Those identified as ambidextrous or did not specify a handedness were excluded from analysis. Videos of each procedure were coded for manual coordination events and coordination duration during the active suture grasping phase. Manual coordination events were defined based on two categories: active motion of dominant, non-dominant, or both hands; and bimanual or unimanual manipulation of instruments during suture grasp attempts. A chi-square test was performed on the number of manual coordination events to discriminate between coordination choices.
Results:Thirty-six residents (52.8% female, 91.7% right-handed) participated in the procedure and met inclusion criteria. Residents used various types of manual coordination during active suture grasping, ranging between 6-26 events (M=14.7, SD=4.5) (see Table 1). Residents switched hands 492 times (M=13.7, SD=4.5). Most of the time was spent using bimanual coordination (M=20.6 seconds, SD=27.2), while unimanual non-dominant coordination was used least (M=7.9 seconds, SD=6.9). As expected, residents did not rely on their dominant and non-dominant hands equally (χ2 (2, N=37)=33.27, p<.001). Only during 22.7% of manual coordination events did residents depend on their non-dominant hand (n=120), which was predominantly used to operate the suture passer device.
Conclusion:Time is frequently used as a metric for surgical experience. Having an understanding of those actions that increase operative time in novices may facilitate training. Our results support the use of focused training to improve hand coordination for bimanual tasks and to improve residents’ use of their non-dominant hand. Future work is necessary to better understand how task completion time and overall performance are affected by residents’ hand coordination during surgical tasks.