J. L. Chan1, Y. Zhou1, M. Li1, J. G. Miller1, S. Wang1, L. C. England2, D. Stroncek2, K. A. Horvath1 1National Institutes Of Health,National Heart, Lung And Blood Institute, Cardiothoracic Surgery Research Program,Bethesda, MD, USA 2National Institutes Of Health,Department Of Transfusion Medicine,Bethesda, MD, USA
Introduction:
Clinical application of stem cell therapy in cardiovascular disease has been performed via intracoronary or intravenous injection, as well as mobilization of bone marrow cells using granulocyte colony-stimulating factor (G-CSF). We report the intramyocardial injection of bone marrow-derived autologous mesenchymal stem cells (MSC) in combination with transmyocardial laser revascularization (TMR) for coronary artery disease patients with depressed left ventricular function.
Methods:
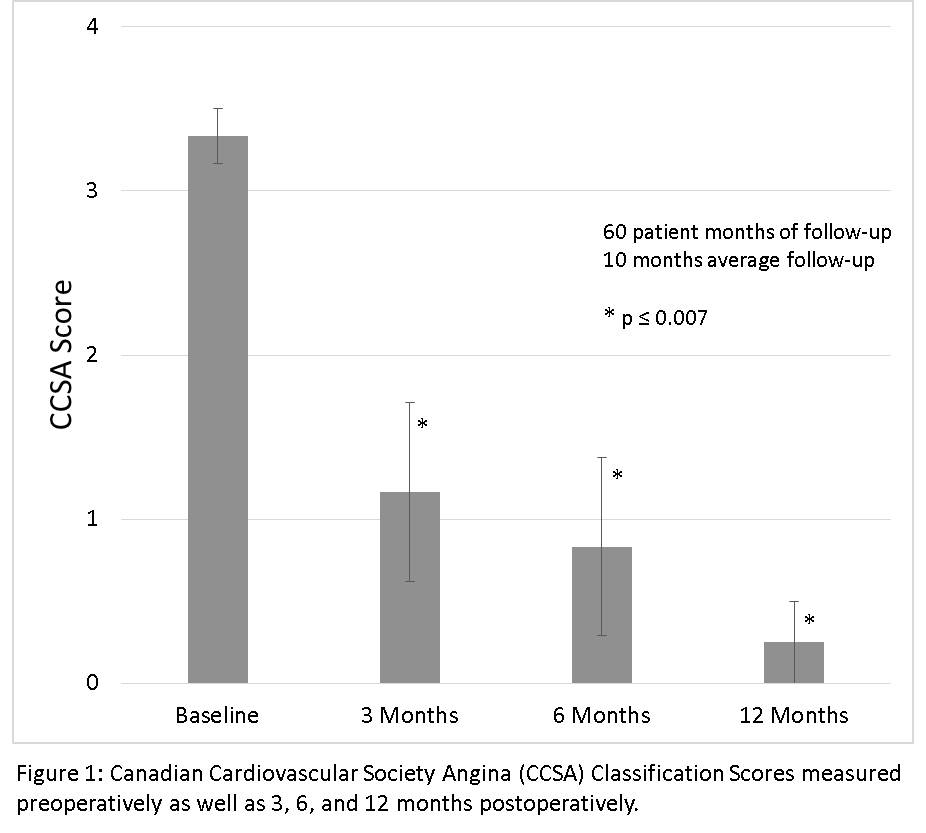
Between April 2012 and May 2015, six patients underwent concurrent TMR and MSC transplantation. To obtain autologous MSCs, bone marrow aspiration was performed three weeks prior to surgery, from which MSCs were subsequently isolated and expanded in vitro. Intraoperatively, MSCs were transplanted into ischemic areas by direct intramyocardial injection (1.5×108 cells) adjacent to TMR channels. Cardiac function was assessed by transthoracic echocardiogram measuring left ventricular ejection fraction (LVEF) and wall motion score index (WMSI) preoperatively as well as three, six, and twelve months postoperatively. Symptomatic improvement was evaluated with the Seattle Angina Questionnaire (SAQ) as well as the Canadian Cardiovascular Society Angina (CCSA) classification system, which were taken at the same time intervals as the echocardiograms.
Results:
Preoperatively, the mean LVEF was 41.26% (95% CI: 36.38%, 46.14%). At three months, LVEF significantly increased by 2.62% (p=0.04), and trended toward continued improvement at six months (+4.24%, p=0.08) and twelve months (+5.22%, p=0.23). Calculated mean WMSI demonstrated superior scores postoperatively at three months (-0.18, p=0.01) compared to baseline (2.16; 95% CI: 1.85, 2.46) and maintains this trend with time (six months: -0.26, p=0.07; twelve months: -0.18, p=0.09). SAQ surveys revealed higher quality of life at 6 months following treatment (+17.64, p=0.02). In comparison to baseline CCSA survey (mean: 3.33, 95% CI: 3.03, 3.70), postoperative CCSA scores indicated significant symptomatic recovery at all time periods (three months: 1.17, p=0.007, six months: 0.83, p=0.003; twelve months: 0.25, p<0.001). With one year follow-up, no major adverse cardiovascular events were observed.
Conclusion:
Intra-myocardial injection of MSCs combined with TMR appears to produce global left ventricular functional improvement as well as symptomatic relief. These findings support the need for additional studies evaluating the efficacy of MSCs during cardiac surgery.