O. A. Lucas1,2, W. Tan1, S. Yendamuri1,2, E. Dexter1,2, A. Picone1, M. Hennon1,2, M. Huang1,2, M. Reid1,3, A. Adjei1,2, T. Demmy1,2, C. Nwogu1,2 2University At Buffalo School Of Medicine And Biomedical Sciences,Buffalo, NY, USA 3University At Buffalo School Of Public Health,Buffalo, NY, USA 1Roswell Park Cancer Institute,Buffalo, NY, USA
Introduction: While others have examined post-operative QOL in NSCLC patients undergoing thoracotomy, similar reports in VATS patients, especially those who received adjuvant chemotherapy, are scarce
Methods: Patients with Stage I or II NSCLC anticipating surgical resection were enrolled in a study using PET probe guidance to detect lymph node metastasis. The Short Form 36 Health Survey (SF-36) assessed changes in patient QOL. The SF-36 was completed by participants pre-operatively and 1, 3, and 6 months post-operatively. A mixed analysis of variance compared scores longitudinally and between groups.
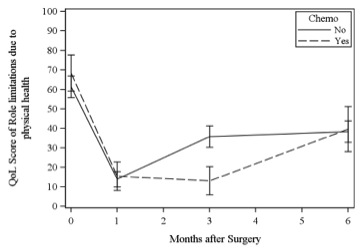
Results:100 patients were enrolled in the study. 88 patients completed the baseline survey and 75 completed at least one post-operative survey. 25 patients received adjuvant chemotherapy following VATS resection and lymph node mapping. Adjuvant chemotherapy started at 1.6 and ended at 3.7 months (medians) after surgery. The trend in overall QOL score between chemotherapy and non-chemotherapy patients was statistically different (p=.004). This difference peaked at 3 months post-operatively (57 vs. 48) and was greatest when comparing role limitations due to physical health (36 vs. 13, p=.028) [Figure 1]. The QOL dimensions significantly impaired by chemotherapy were physical functioning (p=.048), energy/fatigue (p=.001), emotional well-being (p=.031), and social functioning (p=.005). The entire surgical cohort (94 VATS and 6 Thoracotomy) had a drop in QOL scores at 1 month post-operatively (48 vs. 65 baseline score, p<.0001), with recovery by month 6.
Conclusion:Adjuvant chemotherapy patients have a longer QOL decline than those receiving no chemotherapy, but scores return to baseline by month 6. These data help physicians set more realistic QOL impact expectations during chemotherapy and surgery discussions with their patients.