B. J. Nejim1, T. Obeid1, I. Arhuidese1, S. Wang1, K. Yin1, J. Canner1, M. Malas1 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA
Introduction: The aim of the study is to evaluate the occurrence of Thoracic Outlet Syndrome (TOS) surgery, clinical presentations, and 30-day post-operative outcomes using a nationally validated prospective database.
Methods: Patients who underwent cervical/first rib resection surgery (FRRS) between years 2005-2013 were identified in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database. TOS types were examined using post-operative ICD-9 diagnosis codes. Chi-square and ANOVA tests were used to estimate the proportions and mean (±SD) values as appropriate.
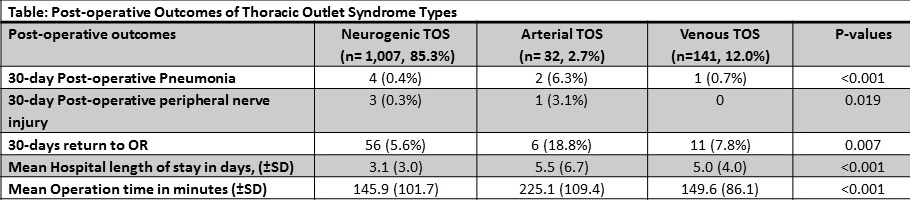
Results: 1,180 patients underwent FRRS during the study period, 1,007 (85.3%) were of the neurogenic type (NTOS), 32 (2.7%) patients had arterial TOS (ATOS) and 141 (12.0%) patients had venous TOS (VTOS). The majority of patients were female (58.3%). Patients with ATOS were significantly older (ATOS: 48.9, ±13.8, VTOS: 35.2, ±11.9 and NTOS: 34.3, ±12.3 years). Overall, 19.3% of the cohort examined were current smokers and this proportion was not different across TOS types (p=0.065). However, among smokers, mean pack-years was higher for patients with ATOS (16.2, ±27.9) compared to NTOS (4.7, ±11.5) and VTOS (3.4, ±11.6) (p<0.001). Mean operation time was over one hour longer for patients with ATOS than for patients with NTOS or VTOS (p<0.001). Average hospital length of stay was longer for patients with ATOS (5.5 days, ± 6.7) (p<0.001). The majority of surgical site infections were superficial (1% of NTOS, 1.4% VTOS and none of the ATOS cases). Post-op pneumonia was proportionally higher in patients presenting with ATOS (6.25%, p<0.001). Post-op peripheral nerve injury was more likely to occur after FRRS for ATOS (p=0.019). Only one patient developed post-operative stroke after FRRS for ATOS. Return to OR within 30 days from the operation occurred in a total of 73 cases (5.6% in NTOS, 18.8% in ATOS and 7.8% in VTOS patients, p=0.007). For the years 2011-2013; all the re-operations were unplanned, with ATOS as the most likely to be re-operated on (p=0.013), readmissions occurred in 33 patients and didn’t differ across TOS types (p=0.525).
Conclusion: Thoracic Outlet Syndrome has been previously studied mainly in highly-experienced single-center contexts. We sought to use NSQIP to further explore its occurrence, types and post-op outcomes at a national level. To our knowledge, this is the first and largest study that represents outcomes of FRRS for TOS from different centers across the United States. Patients underwent FRRS due to ATOS had the highest rates of complications. Further studies are warranted to compare real-world outcomes to highly specialized centers.