M. B. Diffley1, L. R. Putnam1,2, A. Hildebrandt1, K. Caldwell1, A. Minzenmayer1, S. Covey1, K. T. Anderson1,2, A. Kawaguchi1,2, D. Pham1,2, L. S. Kao3, K. P. Lally1,2, K. Tsao1,2 1University Of Texas Health Science Center At Houston,Pediatric Surgery,Houston, TX, USA 2Children’s Memorial Hermann Hospital,Pediatric Surgery,Houston, TX, USA 3University Of Texas Health Science Center At Houston,General Surgery,Houston, TX, USA
Introduction: The effectiveness of surgical safety checklists (SSCs) in reducing post-operative morbidity and mortality is difficult to measure when these outcomes are rare, as in pediatric surgery. However, SSCs may have additional benefits. Good catches and near misses are defined as events which can lead to patient harm but are prevented from occurring. We hypothesized that SSCs increase good catches and near misses.
Methods: A direct observational study from May-July 2015 was conducted. During the performance of the 19-point, pre-incision phase of the SSC, five trained observers documented checklist adherence and good catch or near miss events. The events were organized into five categories by a patient safety expert: communication failures, medication issues, equipment issues, process issues, and safety issues. Regression analysis was used to evaluate the association between events and the performance of the checklist (adherence to all checkpoints), surgical specialty and case duration. Inter-rater reliability (kappa) was determined for checklist adherence.
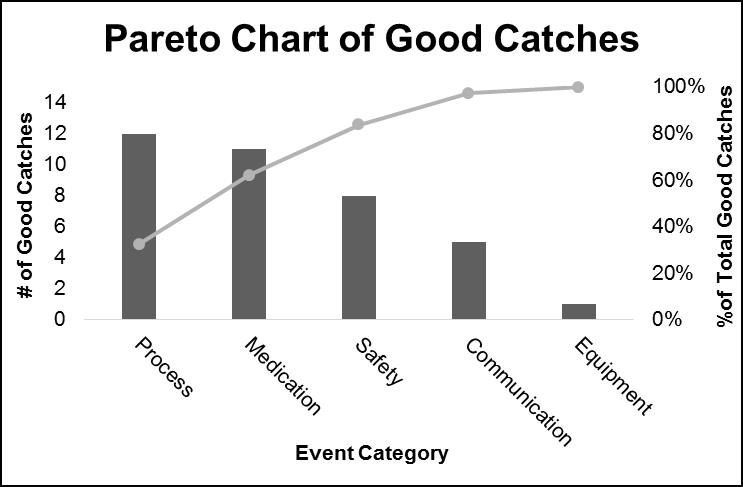
Results:Among 212 cases from 9 pediatric surgical subspecialties, SSCs resulted in detection of at least one event in 37 (17%) cases. The most common events were related to process issues (32.4%); the least common events were due to equipment issues (2.7%, Figure). Median (range) pre-incision checkpoints completion was 18 (7-19). Pediatric cardiovascular surgery cases had the highest event rate of 33%: one good catch or near miss for every 3 cases. Kappa for the pre-incision checklist was 0.70 (95%CI 0.63-0.88). On regression analysis, there were no significant associations between the number of events per checklist and checklist adherence, surgical specialty, or case duration. The median number of events did not vary with case length (<30 min = 1, 31-60 min = 1, 61-120 min = 1, >121 min = 1).
Conclusion: Surgical safety checklists, when performed with high fidelity, can detect good catches and near misses. Evaluation of SSCs often focuses only on morbidity and mortality, while good catches and near misses are not reported. Identification and categorization of these events should be routinely measured since they provide targets for focused quality improvement which may lead to reduced errors and adverse events.