S. I. Feld1, S. E. Tevis1, A. G. Cobian2, M. W. Craven2, G. D. Kennedy1 1University Of Wisconsin,Department Of Surgery,Madison, WI, USA 2University Of Wisconsin,Department Of Biostatistics And Medical Informatics,Madison, WI, USA
Introduction:
Patients who suffer from post-operative complications have longer hospital stays, higher rates of readmission and mortality, and higher cost of care. Many studies have evaluated predictors of complication development. The goal of this study was to assess the temporal relationships among post-operative complications. Knowledge of these relationships will improve our ability to select targeted interventions to prevent cascades of these complications.
Methods:
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database includes preoperative risk factors, intraoperative variables and 30-day postoperative outcomes for patients who underwent major inpatient and outpatient surgical procedures. This study includes cases from this database from 2005 – 2013. Data included all ACS NSQIP-defined complications within 30 days post operation. Machine learning methods were used to model the temporal dependencies between complications. A Markov chain model was developed to model the development of subsequent complications given knowledge of the complications a patient has experienced.
Results:
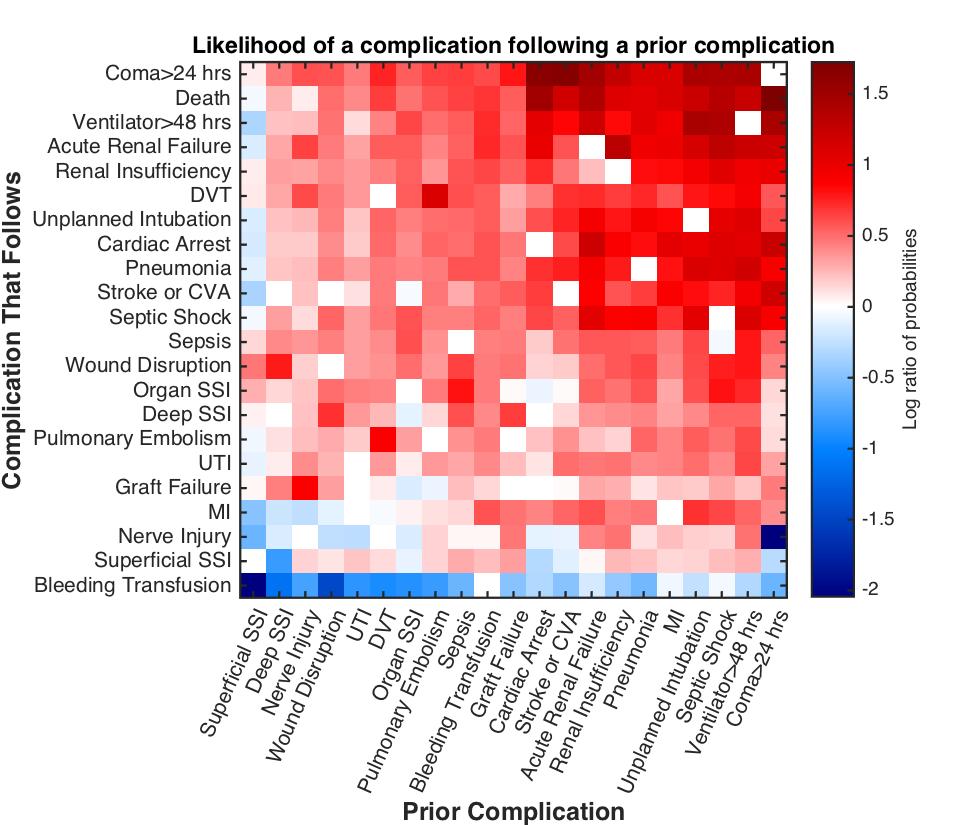
The model was best at predicting death, coma longer than a day, cardiac arrest, septic shock, renal failure, pneumonia, unplanned re-intubation, longer than 2 days on a ventilator and bleeding transfusion (greater than 75% sensitivity at the 75% specificity threshold). The risk for later complications depends on the complications a patient has experienced. We found some complications to be more likely to occur in insolation while others are likely to be associated with a second. Figure 1 shows the risk for complications given a prior complication (normalized by the overall likelihood of diagnosing that complication), with red indicating greater risk and blue less risk than baseline. Complications such as cardiac arrest or MI, renal insufficiency or failure, stroke, intubation, septic shock and coma contributed to complication cascades to a much greater extent than other complications. For example, a patient who has a coma has on odds ratio of >2 of dying within 30 days of the operation while the odds ratio for death following a diagnosis of pneumonia is <0.5.
Conclusions:
A Markov Chain Model combining information about prior complications and time to occurrence after surgery can inform the likelihood of future complications. The present study utilized a novel method to determine several associations among post-operative complications which will contribute to our ability to better target interventions for high-risk post-operative patients.