L. Martin1, S. Finlayson1, B. Brooke1 1University Of Utah,Surgery,Salt Lake City, UT, USA
Introduction:
Transitions of care before and after surgery are a critical time for patients to gain essential information to ensure they understand surgical care plans, avoid adverse events and receive the best outcomes. This study was designed to evaluate how patients prepare for transitions of surgical care, and to explore the association between utilization of health information resources with readmission.
Methods:
A cross-sectional survey was conducted in March 2015 among nationwide members of Health Alliance web-based social communities who reported having direct experience with surgery as either a patient or caregiver. Respondents were asked to report on how prepared they were for the transition of care before and after their most recent surgery, what health information resources they used to get prepared, and whether they required readmission within 30-days following surgery. Survey results were analyzed using bivariate methods.
Results:
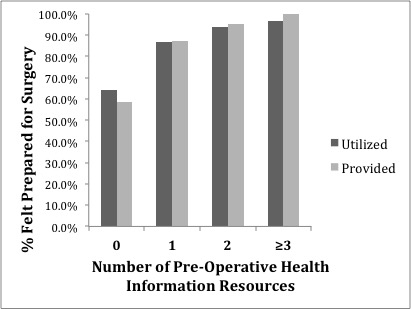
Of 1872 surveyed individuals, 93% were patients and 79% had undergone surgery within the past year. Respondents’ exposure to surgery represented a broad spectrum of ten major disciplines with Orthopedic (28%) and General Surgery (14%) being most common. The majority of respondents felt very prepared prior to undergoing surgery (64%) and before leaving the hospital after surgery (65%). As compared to patients who reported being unprepared, those who felt prepared for transitions of surgical care were most likely to be given multiple health information resources before surgery (97% vs. 79%, p=<0.001) and before leaving the hospital (91% vs. 85%, p=0.02), which included face-to-face meetings, written instructions, internet sites, videos, and smartphone applications. Feeling prepared was significantly associated with the number of resources that patients were provided by their surgical team and used before surgery (Figure 1) and before leaving the hospital. 30-Day readmission was significantly lower among patients who felt prepared either before (8% vs. 23%; p=<0.001) or after surgery (9% vs. 23%, p=<0.001). Furthermore, use of any post-operative resource was associated with a significantly lower 30-day readmission (10% vs 31%, p=<0.001) as compared to patients who reported no health information utilization.
Conclusion:
Patients who report using more health information resources before and after surgery felt more prepared for transitions of surgical care and have a lower rate of 30-day readmission. Ensuring that patients have access to multiple sources of health information and feel prepared for transitions of surgical care is critical to patient satisfaction and obtaining the best clinical outcomes.