D. Z. Semaan1, A. P. Meka1, T. Jaffe1, J. Papin IV1, U. Okoro1, C. Hwang1, A. J. Mullard1, D. Campbell1, M. Englesbe1 1University Of Michigan,Department Of Surgery,Ann Arbor, MI, USA
Introduction:
Surgical site infections (SSIs) following colectomy are morbid and expensive. Previous studies within the Michigan Surgical Quality Collaborative (MSQC) have led to the implementation of a six-element perioperative care bundle for colectomy. The aim of this study was to determine the value (quality and cost) implications of implementation of these bundled perioperative care measures in Michigan.
Methods:
We identified 3,387 patients in the MSQC database who underwent colon surgery from 2012 to 2015. The patient population was stratified into two groups based on compliance: low compliance for adherence to 0-2 perioperative care measures and high compliance for adherence to 3-6 perioperative care measures. Factors potentially associated with SSI were tested using univariate statistical tests. Payment data (patient level) was aggregated in collaboration with Blue Cross Blue Shield of Michigan. Model adjustment covariates included patient demographic factors, clinical factors, case mix, and clustering of patients within hospitals. Adjustments were made to payments to manage hospital-level contractual differences in BCBSM episode payments. A hierarchical generalized linear model was created to test for independent associations between perioperative care measures, SSI and cost.
Results:
The high compliance and low compliance group had risk-adjusted SSI rates of 8.2% (95% CI, 7.21-9.2%) and 16.0% (95% CI, 12.9-19.1%), respectively. This correlates to an absolute risk reduction of 7.8% (p<0.01).
When compared with low compliance, the high compliance group had an absolute risk reduction of 3.6% (p<0.01), 2.9% (p<0.01) and 1.3% (p<0.01) for SSI rates in superficial space, deep space, and organ space, respectively.
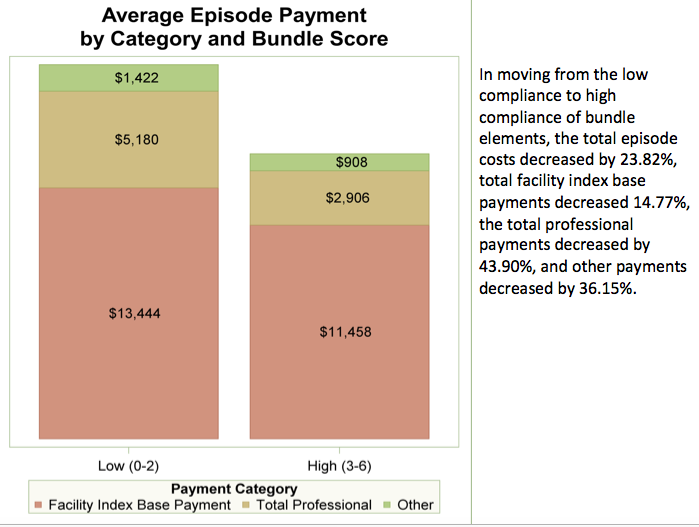
Low compliance cases had an average episodic cost of $20,046 (95% CI, $17,281-$22,812) while high compliance cases had a total episodic cost of $15,272 (95% CI, $14,354-$16,192). This showed a $4,474 (95% CI, $1,859-$7,688) reduction in cost with high compliance cases (p<0.01). Included in this decrease is a $1,986 (14.8%) reduction in facility base payment and a $2,274 (43.9%) reduction in total professional payment. (Figure)
Conclusion:
High compliance with bundle elements shows a statistical reduction in surgical site infections and episode costs. The largest domain of cost savings is professional fee payments. Further implementation of perioperative care bundles will improve the value of colon surgery in Michigan.