J. S. Abelson1, H. Yeo2, J. W. Milsom2, A. Sedrakyan3 1Weill Cornell Medical College,Department Of Surgery,New York, NY, USA 2Weill Cornell Medical College,Division Of Colon And Rectal Surgery,New York, NY, USA 3Weill Cornell Medical College,Division Of Comparative Effectiveness And Outcomes Research,New York, NY, USA
Introduction: Stenting for malignant large bowel obstruction (MLBO) has been used for palliation and bridge to surgery. There is little data comparing stenting to other interventions in a ‘real world’ setting. We report 90-day outcomes using a large database.
Methods: The NY State Department of Health SPARCS database was used to identify patients with emergency treatment for obstructing colon cancer. There were 4 relevant management groups: Group 1(stenting alone); Group 2(stenting followed by resection within 14 days;’bridge to surgery’); Group 3(primary resection with anastomosis); and Group 4(stoma creation with or without resection). Outcomes were major complications, readmission, reoperation, mortality, LOS, and discharge disposition.
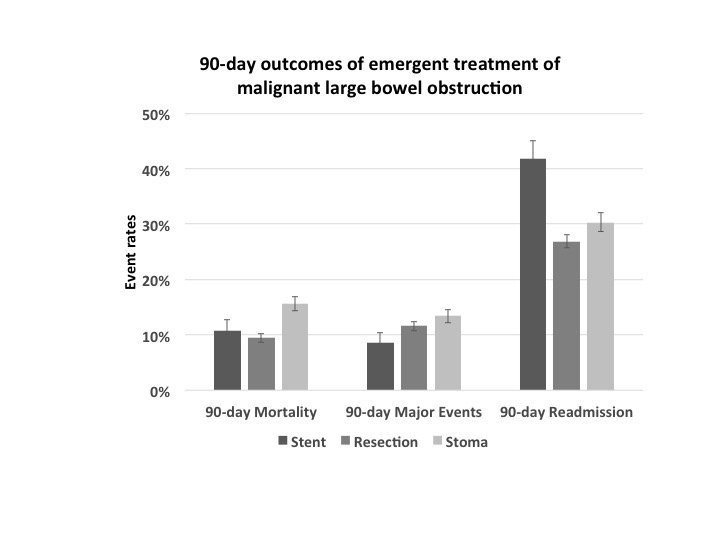
Results: 2,435 patients were treated for MLBO from Oct. 2009 to Dec. 2013. 235 patients underwent stenting alone (Group 1). 57 patients had stenting as their initial procedure followed by resection within 2 weeks (Group 2). 1,388 patients had a primary resection with anastomosis (Group 3) and 755 had a stoma creation (Group 4). Group 2 had a trend towards better outcomes; given the small number (n = 57) and inability to reach statistical significance, these patients were removed from analysis. Among the remaining 3 groups, there were no statistically significant differences between age, gender, or comorbidity but whites were more likely to undergo primary resection (58.8%, 33.1%, 8.1%, p=0.01). High volume centers were more likely to perform stenting compared to low volume centers (19.4% vs 3.5%;p<0.01). LOS was shortest in the stent group (8 days vs 12 days (group 3) and 13 days (group 4); p<0.01) There were no differences in major complication rates between Group 1, 3, and 4 during the index hospitalization and 90 days post-procedure. Patients in Group 1 had the highest rate of 90-day readmissions compared to Group 3 and 4(42.6% vs 26.9% and 30.3%;p<0.01). The percent of patients who underwent reoperation within 90 days in Group 1, 3, and 4 was 17.0%, 2.7%, and 4.0% respectively(p<0.01). The 90-day mortality rate was highest in Group 4 followed by Group 1 and 3(15.6%, 10.6%, 9.4%; p<0.01). Patients in Group 1 were more likely to be discharged to hospice (7.6%) as compared to Group 4 (3.6%) and Group 3 (1.5%) (p<0.01).
Conclusion: Stenting remains an uncommon intervention for patients admitted and treated emergently for MLBO. Not surprisingly, it is most commonly performed at high volume centers, perhaps due to access to advanced endoscopy. The lack of widespread adoption of this intervention could be due to higher 90-day readmission and reoperations rates compared to surgical treatment and use predominantly in high volume centers.