V. Chang2,3, A. N. Kothari1,2, R. M. Yau2, J. M. Albright1, S. Besser5, R. H. Blackwell2,4, G. N. Gupta2,4, P. C. Kuo1,2 1Loyola University Medical Center,Department Of Surgery,Maywood, IL, USA 21:Map Surgical Analytics Research Group,Maywood, IL, USA 3Loyola University Chicago Stritch School Of Medicine,Maywood, IL, USA 4Loyola University Medical Center,Department Of Urology,Maywood, IL, USA 5Depaul University,College Of Computing And Digital Media,Chicago, IL, USA
Introduction:
While many healthcare policy analysts claim that hospital consolidations benefit both health system financial health and patient care by lowering cost and improving quality, very little can be found in literature that examines the latter claim. With more hospital consolidations as an inevitable part of our future healthcare ecosystem, we investigated the relationship between hospital consolidations and surgical outcomes. We hypothesize that hospital consolidations improve surgical outcomes.
Methods:
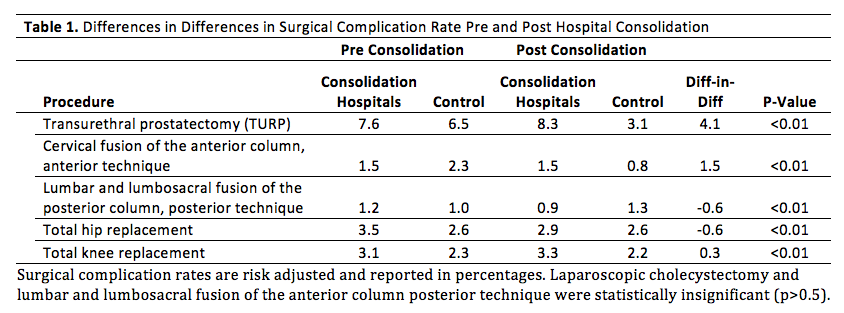
We conducted a retrospective study spanning 2007-2013 in the states of CA and FL using the Healthcare Cost and Utilization Project State Inpatient Database, AHA Annual Survey Database, and Medicare’s Case Mix Index data. We identified 19 hospitals that consolidated over the study period and propensity matched the 19 hospitals with 19 independent hospitals using patient and hospital characteristics. Differences-in-differences analysis was used to compare the change in the risk-adjusted complication rate of 7 elective surgeries 1 year prior to consolidation and the year following consolidation between the consolidation hospitals and matched control group. Our complication index included post-op pulmonary failure, MI, renal failure, PNA, DVT, PE, SSI, hemorrhage, and GI bleed. Based on ProPublica’s surgeon scorecard, the elective surgeries included laparoscopic cholecystectomy, transurethral prostatectomy, cervical fusion of the anterior column (anterior technique), lumbar and lumbosacral fusion of the anterior/posterior column (posterior technique), total hip replacement, and total knee replacement.
Results:
Of the 7 procedures studied, 2 procedures saw a decrease in complication rate (lumbar and lumbosacral fusion of the posterior column posterior technique, DID=-0.6, p<0.01; total hip replacement, DID=-0.6, p<0.01), 3 procedures saw an increase in complication rate (TURP, DID=4.1, p<0.01; cervical fusion of the anterior column anterior technique, DID=1.5, p<0.01; total knee replacement, DID=0.3, p<0.01), and 2 procedures saw no change in complication rate (laparoscopic cholecystectomy, lumbar and lumbosacral fusion of the anterior column posterior technique, both p>0.05) following a hospital consolidation.
Conclusion:
Arguments have been made that consolidated health care systems can share high-performing clinical services and infrastructure resources such as electronic medical records to improve quality. Our results indicate that hospital consolidations result in improved outcomes, but not uniformly. Undoubtedly, many factors affect surgical outcomes following consolidation, such as volume, hospital perioperative resources, reason for consolidating, leadership, and physician factors.