J. D. Rueda1, A. Ruiz Patiño2 1University Of Maryland,School Of Pharmacy,Baltimore, MD, USA 2Hospital Universitario San Ignacio,Bogota, DC, Colombia
Introduction:
Congestion in the postanesthesia care unit (PACU) leads to formation of a waiting queue for patients transferred after surgery. As patient recovery is performed in the operating room, incoming surgeries are delayed. The purpose of this study was to establish the impact of this phenomenon on surgical lost time and finantial resources.
Methods:
An operational mathematical study based on the queuing theory was performed. Average queue length and average hourly queue waiting time were evaluated. Calculations were based on mean patient daily flow, PACU length of stay, occupation and current number of beds. Data was prospectively collected during a period of two months and the variables entry and exit time were recorded for each patient taken to the PACU. Data were imputed in a computational model made with MS Excel®. To account for data uncertainty, a series of deterministic sensitivity analyses for all independent variables were performed.
Results:
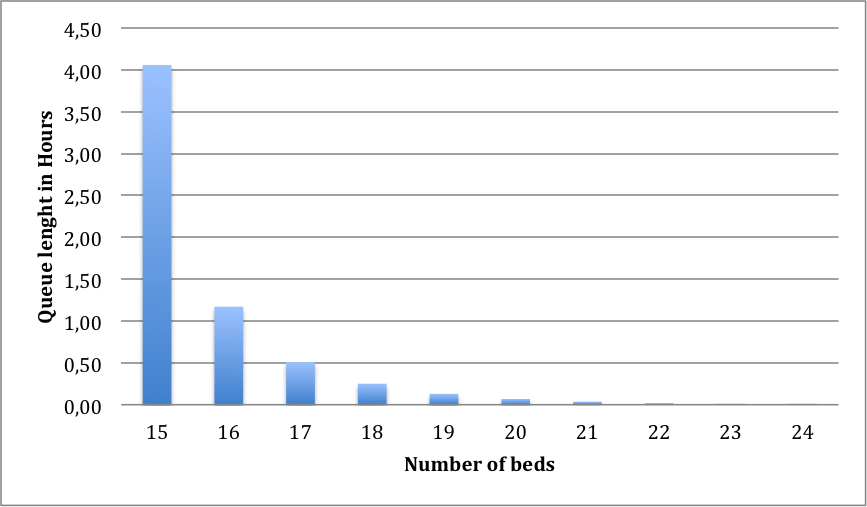
With a mean patient daily flow of 40.3, an average PACU length of stay of 4 hours 25 minutes and 15 beds, average total lost surgical opportunity time, based on occupation analysis, was estimated at 2.36 h (CI95%0.36 – 4.74h). Lost of potential surgical hour equals $1,592. Sensitivity analysis (Figure1) shows that an increase of 2 beds (investment cost of $18,234) is required to solve queue formation.
Conclusion:
Guided by queuing theory, solving congestion in the PACU could lead to an increase in number of daily surgeries and a better cost-opportunity relationship compared to the current capacity.