N. Nagarajan1, K. Giuliano1, J. K. Canner1, C. Wolfgang1, T. M. Pawlik1, S. Terezakis2, J. Herman2, E. B. Schneider1, N. Ahuja1 1Johns Hopkins University School Of Medicine,Surgery,Baltimore, MD, USA 2Johns Hopkins University School Of Medicine,Radiation Oncology,Baltimore, MD, USA
Introduction:
Retroperitoneal sarcomas (RPS) are rare tumors that can be locally aggressive with high rates of recurrence. Given that data on survival of patients with RPS are conflicting, we sought to use a nationwide cancer database to define factors associated with survival in patients with RPS.
Methods:
The Surveillance, Epidemiology and End-Results (SEER) database was utilized to identify patients with RPS from 2002 to 2012. Univariable and multivariable survival analysis was performed using Cox proportional hazard models. Since the underlying hazard function was not proportional, a relative time (Time Ratio) to event (cause-specific mortality) was modeled using a generalized gamma parametric survival function. Exposures of interest included age, sex, race, anatomical region, histological type (using ICD-O-3 codes), grade, size, local extension, lymph node and distant metastases, surgery, and radiation. Choice of appropriate modeling technique was based on Akaike Information Criteria (AIC) values.
Results:
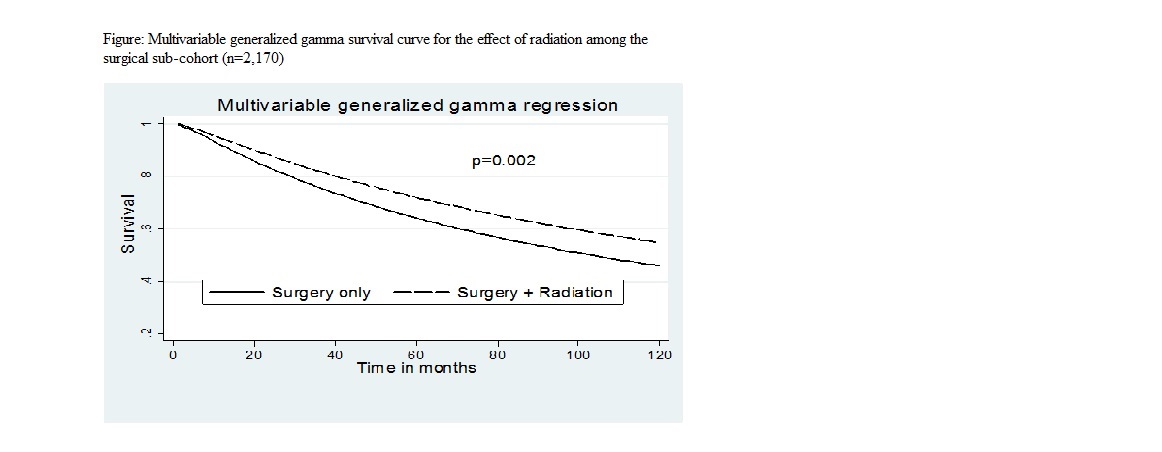
A total of 2,920 patients were included; median age was 63 (IQR: 52-73) years, and 51.6% were female. The most common histological subtypes were liposarcoma (46.9%) and leiomyosarcoma (25.0%). The majority of tumors (84.5%) were <5 cm in size, 42.3% were high grade, and 39.5% had extension to adjacent organs/structures. About three quarters (75.6%) of patients underwent surgical resection, 25.9% had radiation therapy, and 21.6% received both. Overall 5- and 10-year survival were 57.1% and 38.9%, respectively. On multivariable survival analysis, increasing age, histological type (leiomyosarcoma, sarcoma not otherwise specified and others, as compared to liposarcoma), higher grade, increasing size, local extension, and presence of lymph node and distant metastasis were associated with increased risk of death (all p<0.05). After controlling for other factors, patients undergoing surgical resection survived 2.5 times longer than patients who did not undergo surgery (95% CI: 2.1-3.0, p<0.001). Patients who received radiation therapy survived 1.4 times longer than patients who did not receive radiation (95% CI: 1.2-1.7, p<0.001). A similar additive benefit of radiation was seen in the sub-cohort of patients who underwent surgery [Time Ratio: 1.4 (95% CI: 1.1-1.7), p=0.002] (Figure).
Conclusion:
Over the last decade RPS patients treated with radiation demonstrate longer survival compared with patients who did not receive radiation. This relationship was observed both among patients undergoing surgical resection, as well as among patients who did not undergo surgery. Further study is needed to fully elucidate the mechanisms that underlie the radiation-related survival benefit observed in this study.