P. R. Varley1, A. L. Gleisner1, S. T. Tohme1, A. P. Chidi1, D. A. Geller1, A. Tsung1 1University Of Pittsburg,Department Of Surgery,Pittsburgh, PA, USA
Introduction: Previous studies have suggested that survival is associated with the number of lymph nodes examined in patients with node-negative adenocarcinoma of the pancreatic head. For this reason current National Comprehensive Cancer Network guidelines recommend examination of at least 11 lymph nodes for accurate staging. In this study we are the first to investigate whether adherence to this guideline by treatment centers is associated with improved patient survival in a large, multi-institutional dataset.
Methods: The National Cancer Data Base from 1998-2012 was queried for patients undergoing pancreatic resection for adenocarcinoma of the pancreatic head. Adherence to NCCN guidelines was measured by calculating the proportion of patients who had at least 11 lymph nodes (LN) examined at a given treatment center. This proportion was subsequently used in a Cox proportional hazards model with shared frailty was used to evaluate its association with patient survival while controlling for random effects at the level of treatment center. Hierarchical linear regression was used to evaluate the influence of treatment center on LN yield following pancreatic resection.
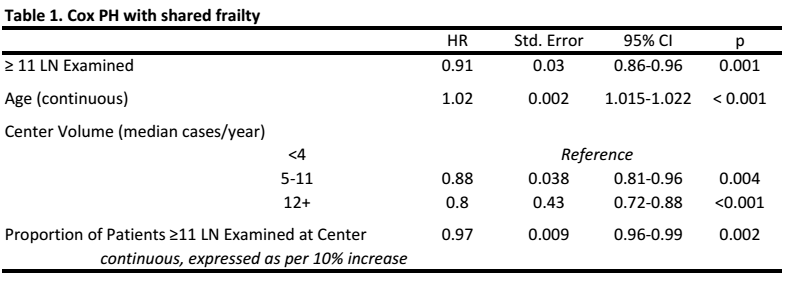
Results: There were 9,247 patients available for analysis. Mean age for the cohort was 66.4±10.8 years. The majority of patients were T3 (54.8%), while 24.3% were T2 and 14.5% were T1. Median yearly treatment center volume ranged from 1 to 86 cases (median 2, IQR 2-4.25). The median proportion of patients having 11 LNs examined at a specific center was 40% (IQR 22.6%-56.7%). Center volume and adherence to the 11 LN guideline were significantly correlated (ρ=0.21, p < 0.001). Centers were divided into tertiles based on adherence, and unadjusted median survival for patients treated at the least adherent tertile was 20.6 months (95% CI 19.5-22.2) and 31.2 months (95% CI 30.0-33.0) at the most adherent. However after adjusting for other covariates and center-specific variation (Table 1), a 10 percent increase in adherence to the 11 LN guideline only revealed a modest association with improved survival (HR 0.97, p = 0.002). Finally in a hierarchical regression analysis clustering within treatment centers accounted for only 15.3% of the variance in the number of nodes examined.
Conclusion: While our results confirm that nodal yield after resection for pancreatic head adnenocarcinoma is associated with survival in node-negative patients, they also show that its utility as a quality metric is limited. Our results confirm the well-described volume-outcome relationship in pancreatic adenocarcinoma and suggest that the survival advantage conferred by treatment at these centers is related to factors unrelated to lymph node yield.