L. V. Selby1, M. B. Rifkin1, M. F. Brennan1, C. E. Ariyan1, V. E. Strong1 1Memorial Sloan-Kettering Cancer Center,Surgery,New York, NY, USA
Introduction: Standardization of post-operative care has been shown to decrease length of stay following colectomy, but has not been evaluated in other complex intra-abdominal operations such as total gastrectomy.
Methods: In June 2009 we instituted a standardized post-operative care pathway emphasizing early oral feeding, early administration of oral pain medication, and early cessation of IV fluids in an attempt to decrease length of stay following total gastrectomy. Patients on pathway receive: clear liquid diet on post-operative day 1, diet progression as tolerated, early oral pain control, and discontinuation of IV fluids when tolerating a post-gastrectomy diet and oral pain medications. Variations of these principles had been employed previously, but not uniformly, among gastric surgeons at our center. We do not routinely place naso-jejeunal tubes or enteral feeding tubes, and only image the esophago-jejeunal anastomosis when clinically indicated. All curative intent gastrectomies performed within two years of standardization were reviewed to determine the effect standardization had on time to oral feeding, oral pain medication, length of stay, complications, and readmissions. Differences between groups were examined using a ranksum test for continuous variables and chi2 test for categorical variables; significance was defined as p <0.05.
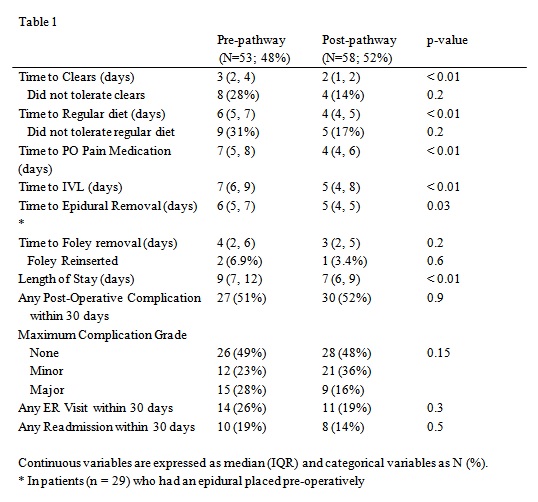
Results: Between June 2007 and July 2011, 111 patients underwent curative intent total gastrectomy, 53 patients prior to standardization (pre) and 58 patients afterwards (post). Patients were predominantly male (70%), median age was 63, median BMI was 27 (pre vs post p = NS). Standardization of post-operative care resulted in a decrease in median time to beginning both a clear liquid diet (pre vs post: 3 days [IQR 2-4] vs 2 days [IQR 1-2]; p < 0.01) and a post-gastrectomy diet (pre vs post: 6 days [IQR 5-7] vs 4 days [IQR 4-5]; p < 0.01), earlier removal of epidural catheters (pre vs post: 6 days [IQR 5-7] vs 5 days[IQR 4-5]; p = 0.03), earlier use of oral pain medication (pre vs post: 7 days [IQR 5-8] vs 4 days [IQR 4-6]; p < 0.01), less time receiving IV fluids (pre vs post: 7 days [IQR 6-9] vs 5 days [IQR 4-8]; p < 0.01), and decreased length of stay (pre vs post: 9 days [IQR 7-12] vs 7 days [IQR 6-9]; p < 0.01). There was no difference between groups in complication rates, complication severity, or the percentage of patients who did not tolerate their diet, returned to our ER, or were readmitted.
Conclusion: Institution of a standardized post-operative clinical care pathway for total gastrectomy was associated with a significantly shorter length of stay with earlier oral feeding without increasing post-operative complication, ER visits, or readmissions.