A. N. Martin1, M. J. Kerwin1, F. E. Turrentine1, T. W. Bauer1, R. B. Adams1, G. J. Stukenborg1, V. M. Zaydfudim1 1University Of Virginia,Department Of Surgery,Charlottesville, VA, USA
Introduction: The impact of transfusion on morbidity and mortality in patients undergoing liver resection has been highly debated. Multiple studies have described worse outcomes associated with blood transfusion among patients selected for hepatectomy. However, independent effects between transfusion and extent of resection have not been well described. We hypothesize that blood transfusion is an independent factor that affects outcomes in patients undergoing hepatectomy.
Methods: Patients at our institution who underwent hepatectomy between 2006 and 2013 were identified and linked with the ACS-NSQIP PUF dataset. Individual abstracted metrics included specific diagnosis and extent of liver resection. Major hepatectomy was defined as resection of > 3 liver segments. Mortality was defined as death occurring within 30 days of the date of surgery. Composite overall morbidity was defined as the occurrence of surgical site infection, wound disruption, pneumonia, unplanned intubation, pulmonary embolism, > 48 hour ventilator, renal failure, urinary tract infection, stroke or cerebral vascular accident, cardiac arrest, myocardial infarction, deep venous thrombosis, or systemic sepsis. The NSQIP estimated probabilities of morbidity and mortality were used to include an overall adjustment for confounding effects, including age and preoperative comorbidities. Multivariable models were used to estimate the effects of extent of resection, estimated probabilities of morbidity and mortality, and use of blood transfusion on 30-day morbidity and mortality.
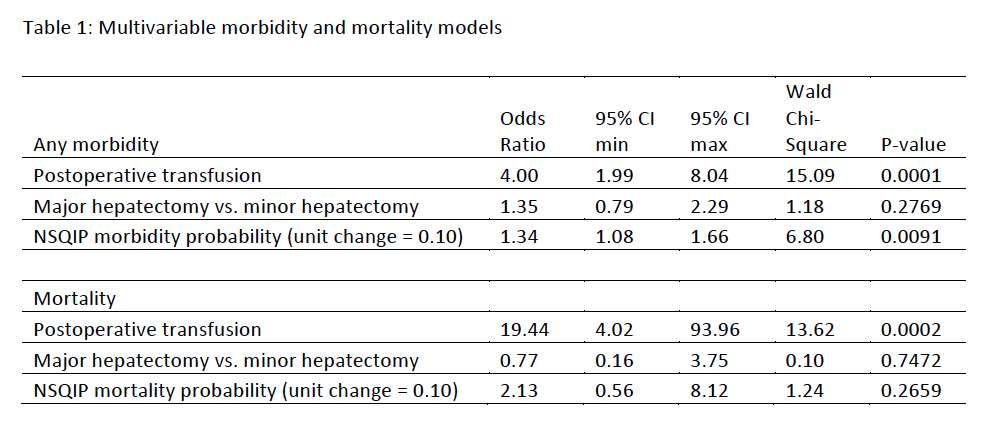
Results: Among 522 patients in the study, 40 (8%) patients required a blood transfusion. 172 (33%) underwent major hepatectomy. Indications for surgery included metastatic neoplasm (n=229, 44%), primary hepatic neoplasm (n=108, 21%), primary extra-hepatic biliary neoplasm (n=23, 4%), and non-malignant indications (n=162, 31%). 86 (16%) patients had a postoperative morbidity; 8 (2%) patients died. After adjustment for significant effect of NSQIP estimated probability of morbidity (OR 1.34, 95% CI 1.08-1.66, p=0.009), blood transfusion was significantly associated with postoperative morbidity (OR 4.00, 95% CI 1.99-8.04, p<0.0001). Extent of resection (OR 1.35, 95% CI 0.79-2.29, p=0.277) was not significantly associated with morbidity. Transfusion was also associated with a significant increase in risk of mortality (OR 19.4, 95% CI 4.02-93.96, p<0.0002). Extent of resection was not associated with mortality in the multivariable model.
Conclusion: Blood transfusion is a highly statistically significant independent predictor of morbidity and mortality after hepatectomy. In patients selected for hepatectomy, extent of resection is not associated with greater risk of postoperative complications.