D. E. Abbott1, C. Tzeng2, M. T. McMillan3, M. P. Callery4, T. S. Kent4, J. D. Christein5, S. W. Behrman6, D. P. Schauer1, M. H. Eckman1, J. J. Sussman1, C. M. Vollmer3 1University Of Cincinnati,Cincinnati, OH, USA 2University Of Kentucky,Lexington, KY, USA 3University Of Pennsylvania,Philadelphia, PA, USA 4Beth Israel Deaconess Medical Center,Boston, MA, USA 5University Of Alabama-Birmingham,Birmingham, Alabama, USA 6University Of Tennessee,Memphis, TN, USA 7University Of Tennessee,Memphis, TN, USA
Introduction: Disease site-specific risk adjustment and predictors of outcome are becoming increasingly useful clinically. However, as payment models for surgical care evolve, it is unclear how such risk stratification may impact patient selection, resource allocation, hospital costs and reimbursements. We sought to determine whether a validated clinical risk score for postoperative pancreatic fistula (POPF) — the most morbid complication following
Methods: A multi-institutional cohort of 1193 patients undergoing PD, POPF risk-adjusted using the validated 10-point Fistula Risk Score (FRS), was matched by clinical outcome with patients undergoing PD at a separate center, from which hospital cost and reimbursement data were utilized. A decision analytic model was constructed to detail the impact of POPF risk, perioperative mortality, complication rates, and readmission rates on hospital costs, payments, and net profits. Probabilistic sensitivity analyses were performed to understand how alterations in clinical variables affected fiscal outcomes.
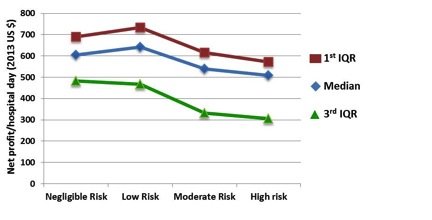
Results: Clinically significant POPF (ISGPF B/C) rates for negligible (0), low (1-2), moderate (3-6) and high-risk (7-10) FRS subsets were 0% (n= 164), 5.2% (n= 343), 16.3%% (n= 603), and 28.9% (n=83), respectively. Per-patient hospital cost for negligible-risk patients was $37,855. Low-, moderate-, and high-risk patients had incrementally higher hospital costs of $38,125 (0.7% above negligible-risk), $41,128 (+8.6%), and $41,983 (+10.9%), respectively. Similarly, hospital payment for negligible-risk patients was $42,685/patient, with incrementally higher payments for low-risk ($43,265; +1.4%), moderate-risk ($45,439; +6.5%) and high-risk ($46,564; +9.1%) patients. Net profit (payment minus cost), however, was similar across incremental risk groups: $4,380, $5,140, $4,311 and $4,581, respectively. The lowest 30-day readmission rates — associated with highest net profit — were also found for negligible/low-risk patients (10.5% and 11.1%), respectively, compared with readmission rates of moderate/high-risk patients (15% and 15.7%, respectively). Net profit per hospital day declined from negligible- to high-risk cohorts – most markedly in patients exceeding median lengths of stay (Figure 1).
Conclusion: Similar to actual POPF rates, financial outcomes following PD can be predicted using a validated clinical risk score for pancreatic fistula. Such accurate risk prediction may help hospitals and payers alike plan for resource allocation, cost controls and reimbursements matched to individual patient risk and acuity.