M. F. Eskander1, S. W. De Geus1, G. G. Kasumova1, S. Ng1, W. Al-Refaie3, G. Ayata2, J. F. Tseng1 1Beth Israel Deaconess Medical Center,Department Of Surgery,Boston, MA, USA 2Beth Israel Deaconess Medical Center,Department Of Pathology,Boston, MA, USA 3MedStar Georgetown University Hospital,Department Of Surgery,Washington, DC, USA
Introduction: Lymph node examination during pancreaticoduodenectomy (PD) is a joint venture between surgery and pathology. Previous studies have suggested that frequently, insufficient lymph nodes are evaluated, leading some patients with N1 disease to misclassified as N0. We examine trends in lymph node dissection over time and investigate whether changes may have impacted overall survival and the long-term prognostic value of lymph node status.
Methods: The National Cancer Data Base was queried for patients diagnosed with non-metastatic pancreatic adenocarcinoma between 1998 and 2012 who underwent classic PD with antrectomy. Patients with unspecified number of lymph nodes examined were excluded. Cochran-Armitage trend analyses were performed to test for linear trends in binomial proportions of node examination and N classification over time. Kaplan-Meier curves and Cox proportional hazards models were used to assess the impact of lymph node status on overall survival for patients diagnosed over 2-year intervals from 1998-2011.
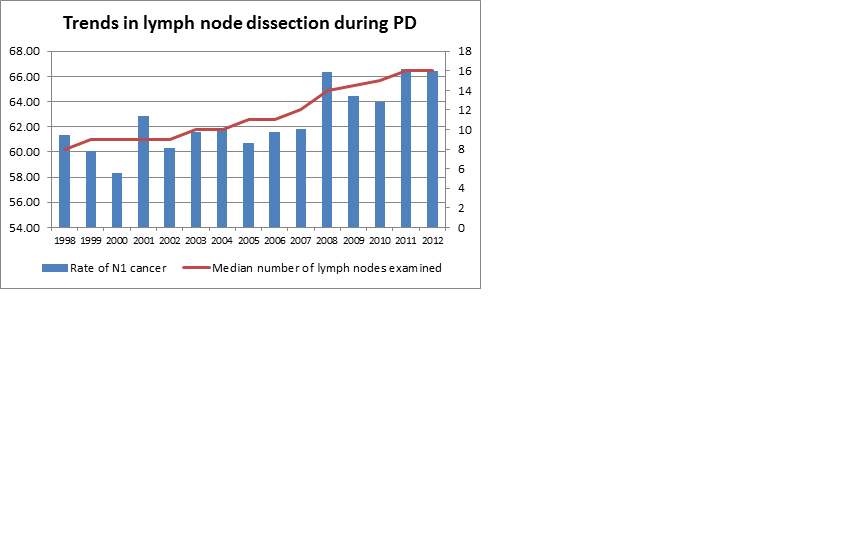
Results: For PDs in which at least one node was surgically examined, the median number of examined lymph nodes nearly doubled from 8 (IQR 5-13) in 1998 to 16 (IQR 11-23) in 2012. The rate of N1 disease increased from 61.3% to 66.4% (p<0.0001). (Figure) Over all years, median LNR remained between 0.10-0.13. 7.3% of resected patients in 1998 had no lymph nodes examined compared to only 2.4% in 2012 (p<0.0001). Median survival was significantly different between N1 and N0 patients (all p<0.0001) at all time intervals, and survival in both subgroups improved. In successive multivariate models adjusted for gender, race, T stage, margin status, and tumor grade, N0 vs. N1 status was consistently protective for overall survival (p<0.0001), but there was no change in the magnitude of its hazard ratio over time (overall HR 0.718; 95% CI 0.696-0.741). Likewise, lymph node status continued to be a significant predictor of overall survival when models were stratified by receipt of chemoradiotherapy vs. chemotherapy only vs. neither (HR 0.690; CI 0.669-0.713) and when stratified by age group (HR 0.709; CI 0.687-0.732).
Conclusion: In contrast to previous years, contemporary patients have an adequate number of nodes examined during standard PD. This, along with with rising rates of N1 cancer detection, suggests more accurate classification of lymph node status and prognosis after resection. However, the strength of lymph node status as a prognosticator for overall survival has not changed. More research is needed regarding the repercussions of increased lymph node dissection and the optimal standards for nodal harvest and evaluation in the modern era.