A. Fingeret1, K. Economopoulos1, Y. Chen1, P. Sadow2, R. Hodin1, S. Parangi1, C. Lubitz1 1Massachusetts General Hospital,Endocrine Surgery Division,Boston, MA, USA 2Massachusetts General Hospital,Department Of Pathology,Boston, MA, USA
Introduction: Papillary thyroid carcinoma (PTC) incidence is increasing, yet disease specific survival has remained largely unchanged. BRAF mutational status has been inconsistently correlated with recurrence. Furthermore, with the impetus to observe low risk tumors without resection, accurate risk stratification is paramount.
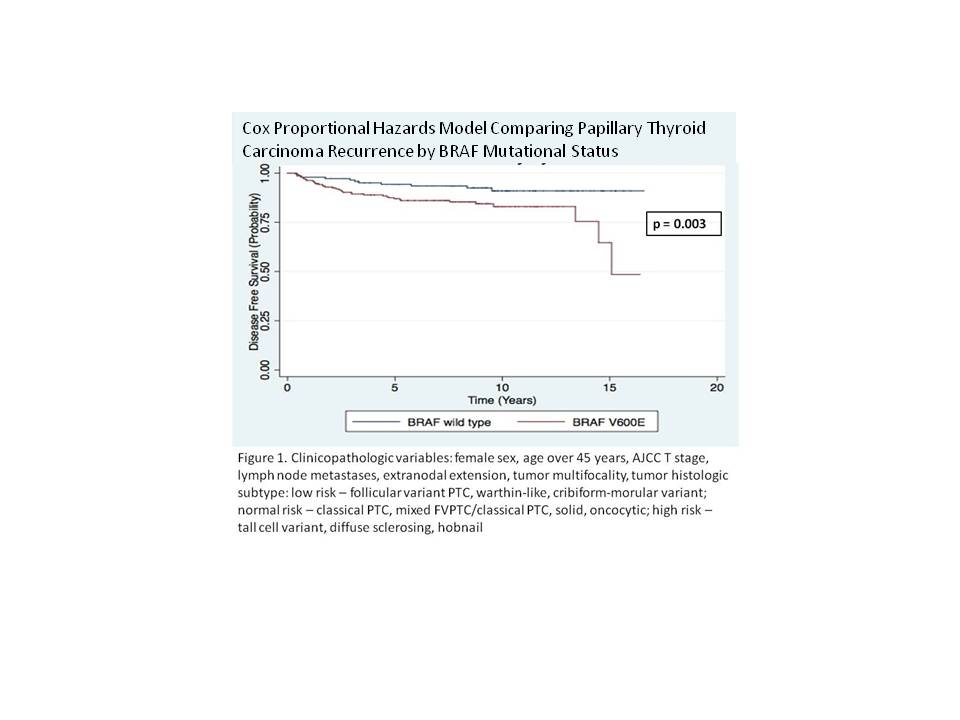
Methods: An unselected historical cohort of patients (from 2000 – 2007) who underwent at least total thyroidectomy for PTC was analyzed to model recurrence by BRAF mutational status. BRAF status was determined by DNA extraction and PCR-based single nucleotide extension genotyping of paraffin embedded primary tumor specimens. Univariate analysis was performed with Wilcoxon rank sum and log rank test. A multivariable cox proportional hazards model was used to determine clinicopathologic factors associated with time to recurrence (primary outcome) and second recurrence (secondary outcome). Recurrence was defined as pathologically confirmed PTC or distant metastases treated with radioactive iodine (RAI) greater than 90 days from index operation.
Results: The recurrence incidence within our 605 patient cohort was 77 (12.7%). Of these, BRAF mutational status was determined for 402 (66.4%) with 254 (63.2%) containing BRAFV600E. The median overall follow up was 8.3 years (IQR 6.6 – 10.3) with 7.7 years (6.0 – 9.3) for BRAFV600E and 8.6 years (IQR 7.0 – 11.0) for wild type.There were no differences in clinicopathological risk factors between patients with and without BRAF testing. The incidence of recurrence among BRAFV600E patients was 38 (17.6%) compared to 11 (8.0%) among BRAF wild type (p = 0.02). Of the initial and repeat recurrences, 76 (98.7%) and 16 (80%) were locoregional, respectively. In the multivariable cox regression analysis controlling for clinicopathologic risk factors (Figure 1), the likelihood of PTC recurrence was increased by BRAF mutation status (hazard ratio 2.4, p = 0.03), tumor size by AJCC T stage (HR 1.9, p = 0.01), and regional lymph node metastases at index operation (HR 1.9, p =0.01). The median time to recurrence overall was 1.9 years (IQR 0.68 – 4.1), 2.1 years (IQR 1.1 – 4.3) for BRAFV600E and 2.8 years (IQR 0.6 – 5.3) for wild type. Twenty patients developed a second recurrence; in this subset of patients the incidence of BRAFV600E was also significantly correlated with time to recurrence (p = 0.04). Eleven (1.8%) patients died, with four (0.7%) deaths attributable to PTC.
Conclusion: Adjusting for known clinicopathologic risk factors for PTC recurrence, BRAF V600E mutation remains predictive over a long follow up.