T. B. Tran1, D. J. Worhunsky1, J. N. Leal1, G. A. Poultsides1, J. A. Norton1, B. C. Visser1, M. M. Dua1 1Stanford University,Stanford, CA, USA
Introduction: In recent years, several institutional reports of robotic distal pancreatectomy (RDP) claim superiority over laparoscopic distal pancreatectomy (LDP) given its ability to overcome technical limitations associated with traditional laparoscopic surgery. However, many of these comparisons include RDP cohorts comprised of smaller subset of surgeons that adopt the robotic platform or 2 attending surgeon teams versus LDP cohorts from larger groups of institutional surgeons across several disciplines. We hypothesize that this difference in surgical teams is a primary contributing factor to the superior outcomes of RDP.
Methods: We performed a retrospective analysis of all minimally invasive spleen-preserving distal pancreatectomies from 2008 to 2015. All cases were performed with the intent to preserve the spleen. Operative characteristics, perioperative outcomes, and 90-day morbidity were compared between LDP and RDP. Subgroup analysis of institutional LDP versus RDP and single-surgeon LDP versus RDP was also performed to control for surgeon variability.
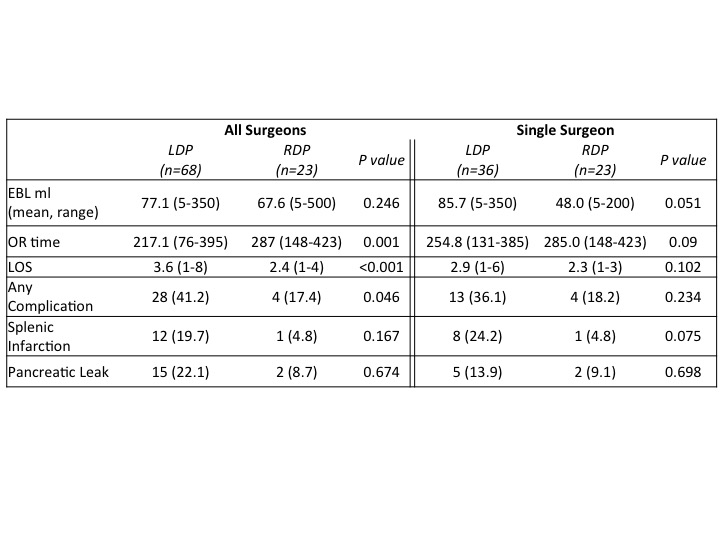
Results: A total of 95 patients underwent minimally invasive distal pancreatectomy with intent to preserve the spleen: 71 (74.7%) LDP and 24 (25.3%) RDP. Conversion rates to open distal pancreatectomy were equivalent (1 RDP and 3 LDP; both 4.2%). Rates of any complication were higher in the LDP group (42.2% vs. 17.4; p=0.046) but specific complications including pancreatic leak, postoperative bleeding, wound infection, intra-abdominal abscess, and splenic infarction were similar between the groups. Although operative time was higher in patients who underwent RDP (mean 287.1 vs. 217.1 min; p=0.001), hospital length of stay was significantly shorter in the RDP group (mean 2.4 vs. 3.6 days; p< 0.001). RDP was associated with more than two-thirds odds reduction in postoperative complications (OR 0.30 95% CI 0.092-0.980; p=0.046). However, subgroup analysis demonstrated that differences between LDP and RDP diminish upon evaluation of single-surgeon outcomes (Table). The previous RDP risk reduction of postoperative complications was not significant in subgroup analysis of a single surgeon who is facile in both RDP and LDP (OR 0.39, 95% CI 0.959-1.041; p=0.98).
Conclusion: RDP is an acceptable minimally invasive approach with postoperative outcomes equivalent to that of LDP in carefully selected patients. Although RDP may offer the benefits of improved range of motion and dexterity over LDP, the novel robotic approach is not necessarily better than LDP as often claimed in institutional comparisons. Robotic technology should be viewed as another tool to facilitate the transition from open surgery rather than a replacement of laparoscopic technique.