N. S. McCall1, C. B. Chen1, M. J. Pucci1, S. Doane1, J. M. Winter1, C. J. Yeo1, H. Lavu1 1Thomas Jefferson University,Department Of Surgery,Philadelphia, PA, USA
Introduction: Postoperative pancreatic fistula (PF) remains one of the most significant complications after pancreaticoduodenectomy (PD). Soft (normal) pancreas texture is a well-established risk factor for PF. Recently, studies have suggested that post-PD serum hyperamylasemia (PPHA) may also be a risk factor. In this study, we evaluate the relationship of pancreas texture and post-operative serum amylase levels in determining PF risk in patients who have undergone PD.
Methods: This retrospective cohort study utilizing the pancreatic surgery database at Thomas Jefferson University evaluated all patients who underwent PD from 2009 to 2014. The highest postoperative serum amylase level from postoperative day (POD) 0 to POD 5 was obtained. An ROC curve analysis obtained a threshold value to define PPHA compared to normal serum amylase levels. Chi-square analyses and odds ratios evaluated the relationship between pancreas texture, serum amylase level, and the development of PF.
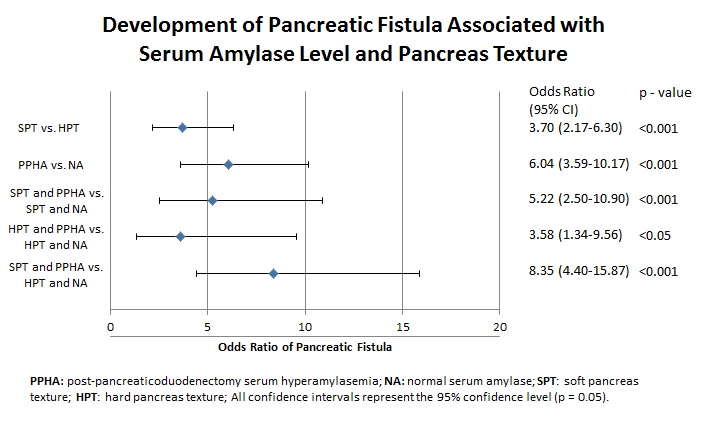
Results: Data from 525 consecutive patients were analyzed after excluding 80 due to a lack of information on pancreas texture. Serum amylase levels on POD2-POD5 were not found to be predictive of PF occurrence; thus, the remaining analysis focused on the highest amylase value between POD0 and POD1. The serum amylase threshold value of 165 IU/I yielded greatest accuracy from the ROC curve analysis (AUC: 0.75; Sensitivity: 0.70; Specificity: 0.72). Demographics and clinical information were similar between patients with PPHA and those with normal serum amylase. Soft pancreata were more likely to have PPHA (p < 0.001) and PF (p < 0.001) than hard pancreata. PPHA was associated with increased rates of PF (p < 0.001), intra-abdominal abscess (p < 0.001), delayed gastric emptying (p = 0.04), wound infection (p < 0.001), hepaticojejunostomy or duodenojejunostomy leakage (p = 0.03), cardiac complications (p = 0.02), pulmonary complications (p < 0.001), as well as increased length of stay (p < 0.001). Fifty-nine patients with soft pancreata developed PF, with 49 (83%) having PPHA. Overall, patients with a soft pancreas and PPHA had the highest PF rate (34.5%), and those with a hard pancreas and normal serum amylase had the lowest rate (5.9%)(Odds ratio: 8.35; 95% CI: 4.4-15.9).
Conclusion: Accurate estimation of PF risk is achievable by incorporation of pancreas texture and immediate post-operative serum amylase levels. Analysis of their interplay segregates patients into well-defined risk groups. The presence of PPHA on POD0 or POD1 increases PF risk, even more so than soft pancreatic texture alone. The minimal PF rate in patients with hard pancreata and normal POD 0-1 serum amylase levels identifies a cohort unlikely to develop PF.