G. C. Ives1, F. R. Demehri1, R. Sanchez2, M. Barrett1, D. H. Teitelbaum1 1University Of Michigan,Department Of Surgery, Section Of Pediatric Surgery,Ann Arbor, MI, USA 2University Of Michigan,Department Of Radiology, Section Of Pediatric Radiology,Ann Arbor, MI, USA
Introduction:
While previous research demonstrated a relationship between achieving enteral autonomy (EA) in pediatric short bowel syndrome (SBS) and anatomy of the remaining bowel, including presence of the ileocecal valve and % predicted small bowel length (SBL) remaining, changes in SB diameter (SBD) are part of a unique adaptive response that may warrant further investigation. However, little is known about the natural history of changes in SBD after SBS, and understanding which children develop this type of adaptation and factors associated with it has important implications, as SBD has been identified as a factor in determining eligibility for an intestinal lengthening procedure (ILP). The objective of this study was to evaluate contributory factors for SBD in SBS patients and the effects of SBD on patient outcomes.
Methods:
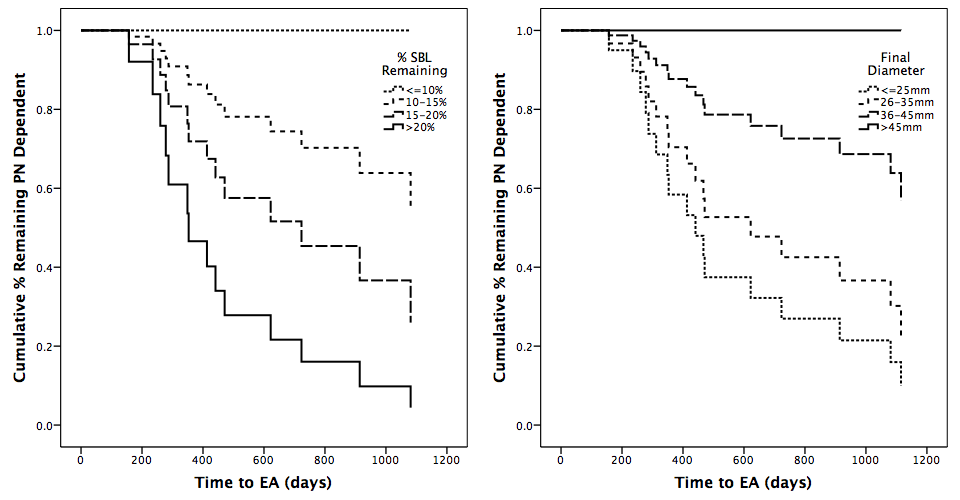
This is a retrospective review of SBS patients (defined as dependence on parenteral nutrition (PN) for >60days secondary to loss of intestinal length) born since 2000. We identified 30 children with adequate imaging to assess SBD at more than one time point following bowel resection and prior to any ILP. Demographic and clinical data were collected and SBD was measured on GI contrast studies by a pediatric radiologist. Studies that demonstrated SB obstruction or stricture were excluded, and diameter was measured relative to vertebral size and compared with proximate calibrated films when necessary. SBL was converted to % predicted length based on gestational age (GA). Analysis of factors associated with EA and SBD in the last scan before end of follow-up or EA was conducted using Fisher’s Exact Test, Student’s t-test, K-M survival analysis, Cox regression, and linear or logistic regression, as appropriate.
Results:
30 children with median GA of 31.5 (IQR 27,35) weeks were followed for 52.6 (28.1,80.4) months. Necrotizing enterocolitis was the most common etiology of SBS (n=13,43%). EA was achieved in 17 (57%), while 11 (37%) remained on PN and 2 (7%) died during follow-up. Median SBD was 23.5mm (IQR 18,42.3), and 9 children demonstrated significant dilation (SBD>40mm,30%). Bivariate analysis identified higher % SBL {OR 1.40)95% CI:1.07,1.83)} and lower SBD {OR 0.87(95% CI:0.80,0.96)} as predictive of achieving EA, and in survival analyses <10% SBL (P=0.024) and higher SBD {HR 0.93(95% CI:0.88,0.98)} predicted increased time to EA. Multivariate linear regression identified lower % SBL {OR -1.02(95% CI:-1.58,-0.45)} and higher birth weight {OR 7.32(95% CI:2.37,12.26)} as strongly predictive of higher SBD.
Conclusion:
SBD is a highly prognostic factor inversely associated with achieving EA in SBS children that can be measured in real-time to track patient progress and inform clinical decision-making.