D. P. Bent1, A. Benedict1,2, J. Nelson2, H. C. Jen1,2 1Tufts University School Of Medicine,Boston, MA, USA 2Tufts Medical Center,Boston, MA, USA
Introduction: Newborns with congenital diaphragmatic hernia (CDH) can have dramatically different mortality rates depending on their presentation. A recently published clinical prediction model from the CDH Study Group (CDHSG) Registry stratified CDHs into low-, intermediate-, and high-risk groups based on birth information and associated anomalies. However, this registry-based prediction model has not been validated externally. The purpose of our study was to examine the validity of this new model on a statewide cohort of newborns with CDH.
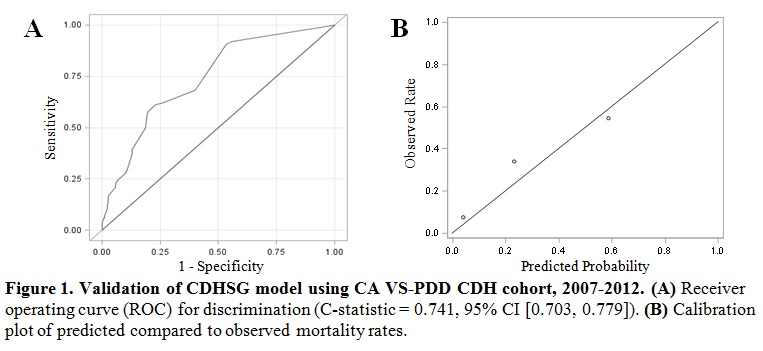
Methods: Newborns with CDH in California between January 1st 2007 and December 31st 2012 were extracted from the Vital Statistics and Patient Discharge Data (VS-PDD) Linked Files. Subsequent patient transfers and discharges before one year of age were tracked via a de-identified birth id. Our primary outcome was survival to discharge during the initial phase of care. Binary independent predictors were generated from birth weight, 5-minute Apgar score, and the presence of pulmonary hypertension, major congenital cardiac and/or chromosomal anomalies. Performance of the CDHSG clinical prediction model (i.e. total CDH score) on our VS-PDD cohort was validated in terms of discrimination and calibration.
Results: There were 3,213,822 live births in California during the study period. We extracted 753 newborns with the diagnosis of CDH, an incidence of ~1/4,250 births. Forty-eight infants (6.4%) were excluded due to incomplete birth information, leaving a total of 705 unique infants with CDH in our study cohort (N=705). The majority was male (58.6%) and the median gestational age, birth weight, and 5-minute Apgar score were 38.7 weeks, 3000 g, and 8 respectively. Pulmonary hypertension was present in 30.1%, while major cardiac and chromosomal anomalies were found in 18.4% and 7.9% of our cohort. CDH newborns in our cohort were delivered in 150 different hospitals, whereas only 28 hospitals performed CDH repairs (1-85 repairs per hospital).
The observed mortality for low-, intermediate-, and high-risk groups according to the total CDH score were 7.7%, 34.3%, and 54.7%, while the predicted mortality for these three risk groups were 4.0%, 23.2%, and 58.5%. The CDHSG model performed well in our cohort with a C-statistic of 0.741 and good calibration (Fig. 1).
Conclusion: We identified the first non-voluntary population-based cohort of CDH newborns in the United States that can be accurately risk stratified using a recent clinical prediction model derived by the CDHSG. This cohort of CDH newborns may be used in the future to investigate hospital volume-outcome relationships, identify ideal resource allocation, and guide policy development for CDH infants in the U.S.