C. K. Zogg1, W. Jiang1, A. A. Shah1,2, J. W. Scott1, E. J. Lilley1, L. L. Wolf1, M. Chaudhary1, L. M. Kodadek3, O. A. Olufajo1, D. Metcalfe1, E. B. Schneider1, Z. Cooper1, A. Salim1, A. H. Haider1 2Division Of General Surgery, Mayo Clinic,Scottsdale, AZ, USA 3Department Of Surgery, Johns Hopkins University School Of Medicine,Baltimore, MD, USA 1Center For Surgery And Public Health, Harvard Medical School & Harvard School Of Public Health, Department Of Surgery, Brigham And Women’s Hospital,Boston, MA, USA
Introduction: As the fastest growing segment of the US population, older adults (≥65y) represent an increasing number of patients requiring emergency surgical (EGS) care. Efforts are needed to understand their unique health needs. Previous studies have found that universal access to insurance mitigates racial/ethnic disparities in younger adults. However, little is known about the role of race/ethnicity in post-discharge outcomes after EGS among older patients. The objective of this study was to determine whether racial/ethnic disparities in outcomes persist among Medicare beneficiaries requiring EGS consultations/care.
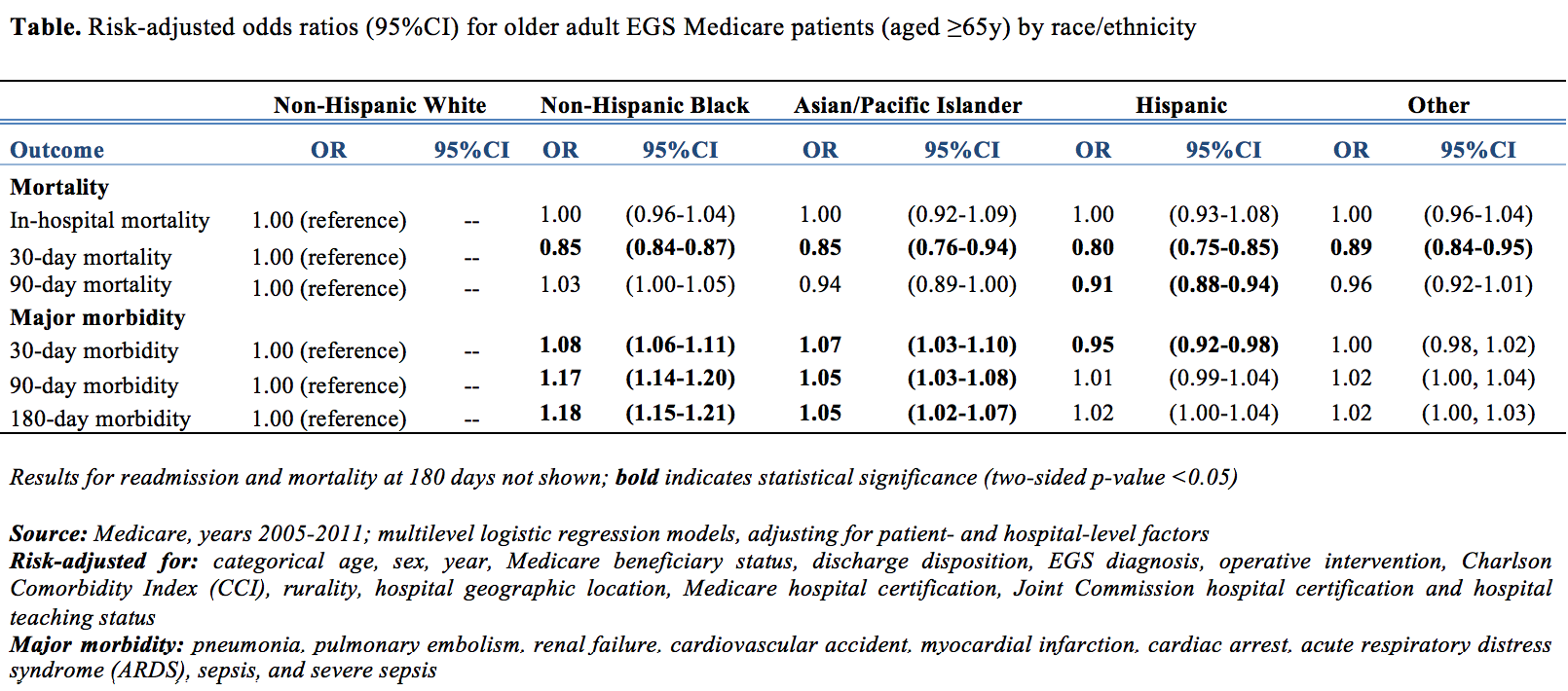
Methods: Seven years (2005-2011) of Medicare data were queried for patients with a primary EGS diagnosis, defined by the AAST, who were admitted to inpatient status through the ED and had racial/ethnicity data recorded for a single race/ethnicity. Associations with demographic, clinical, and hospital-level factors were considered using descriptive statistics. Risk-adjusted multilevel logistic regression assessed differences in in-hospital mortality and mortality, major morbidity, and readmission rates at 30, 90, and 180 days. Differences in discharge disposition, including utilization of hospice or rehabilitation, were also considered.
Results: A total of 7,763,510 patients were identified: 85.5% White, 9.6% Black, 2.1% Hispanic, and 1.1% Asian/Pacific Islander. Older adults were approximately evenly distributed across 5-year increments of age (15.2-19.6%) with 9.9% (n=770,560) aged ≥90y. One-fifth (22.2%) was managed in the ICU (1.0% surgical; 9.9% general), and 32.7% had a CCI ≥3. Overall risk-adjusted outcomes are presented (Table). Worse outcomes among older minority patients were not consistently found; differences in mortality decreased, while disparities in morbidity/readmission paradoxically remained. Stratification by diagnostic group and among patients restricted to octogenarian/nonagenarians – known to experience different outcomes than younger geriatric patients (65-80y) – revealed similarly mixed associations.
Conclusion: Lack of significant differences for in-hospital/90-day mortality and protective effects reported at 30 days between Black and White patients suggest that enhanced insurance coverage of emergency surgical care among older adult patients is associated with mitigation of racial/ethnic disparities. Akin to older trauma patients, who show lower inpatient mortality for Black versus White patients, older adult EGS patients demonstrate persistent differences between Black and White patients in longer-term (30/90/180-day) survival that extend well beyond index hospital stays. Ongoing efforts are needed to understand the persistence of disparities in morbidity and readmission rates.