C. Jones1, A. Gullick1, D. I. Chu1, B. Pearce1, M. Morris1 1University Of Alabama – Birmingham,Department Of Surgery,Birmingham, AL, USA
Introduction:
Readmission rates following vascular surgery are among the highest within surgical specialties, and lower extremity bypass has the highest readmission rate of vascular surgery procedures. Understanding risk factors for and ultimately predicting readmission within this population could have significant clinical impact. We hypothesize that readmission rates following lower extremity bypass differ based on the indication for surgery.
Methods:
We queried the 2012-2013 American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) procedure targeted vascular cohort to identify all patients who underwent lower extremity bypass. Patients were stratified by surgical indication: Aneurysm, Claudication, Critical limb ischemia rest pain, Critical limb ischemia tissue loss, or Other. Patients with a postoperative length of stay greater than 30 days or death within 30 days were excluded. Chi-square and Wilcoxon Rank Sums tests were used to determine the differences among categorical and continuous variables, respectively. The primary and secondary outcomes were unplanned readmissions and postoperative complications, respectively. Predictors of readmission were identified with logistic regression using a negative binomial model, and multivariable analysis was used to adjust the odds ratio of readmission for surgical indication.
Results:
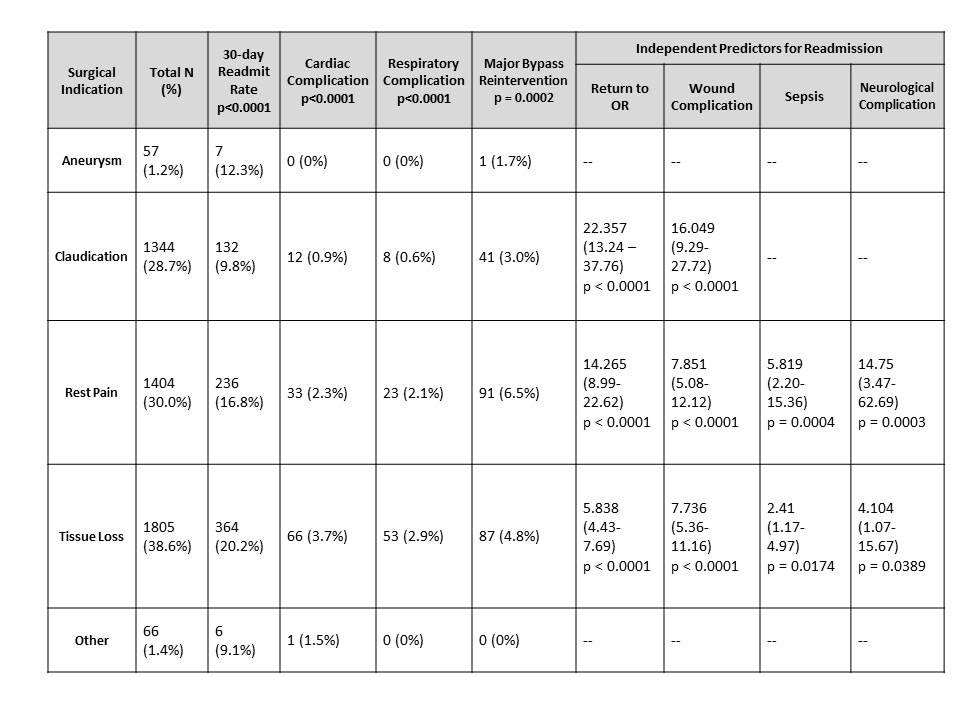
Of the 4,676 lower extremity bypasses that were performed, 94.1% were elective and 5.1% were emergent. The cohort consisted of 65.2% males, 34.8% females, 72.2% whites, and 16.5% blacks. The overall 30-day readmission rate was 15.9%. Readmission rates varied significantly based on the indication for surgery. On unadjusted comparison, 20.2% of patients with tissue loss were readmitted compared to 16.8% with rest pain, 12.3% with aneurysms, and 9.8% with claudication (p<0.0001). Unadjusted postoperative cardiac and respiratory complications as well as major bypass reinterventions varied significantly based on surgical indication (Table). Significant adjusted odds ratios of readmission were 1.617 for tissue loss versus claudication (p=0.0003) and 1.533 for rest pain versus claudication (p=0.0013). Several odds ratios for readmission based on adjusted predictors of readmission were significant for surgical indications (Table).
Conclusion:
The risk for readmission after lower extremity bypass and postoperative complications vary significantly based on the surgical indication. All lower extremity bypasses are not performed for one diagnosis. If hospitals are to be penalized for high readmission rates, then the readmission rates following lower extremity bypass should be adjusted for surgical indication.