J. Biggs1, S. Barnes1, S. Osterlind1, E. Dalton1, L. Hanley1, S. Ahmad1 1University Of Missouri,Surgery,Columbia, MO, USA
Introduction:
The management of peptic ulcer disease (PUD) has evolved from a primarily surgically managed disease to a medically managed one with advances in endoscopic therapies and treatment of H. pylori infection. While the incidence of hospital admissions for PUD may have changed over the decades, ulcer disease remains a significant cause for mortality, with perforation having a mortality of approximately 11-16%, and morbidity of approximately 30%. The incidence of acute perforation of PUD remains around 4-11 cases per 100,000/year and is the most common etiology for pneumoperitoneum identified on radiography. We utilized the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database Participant User File (PUF) to study preoperative, demographic and postoperative variables that may be associated with morbidity and mortality after emergent surgical management of acute perforated PUD.
Methods:
The adult ACS-NSQIP database participant user files were queried from 2005 to 2013. Those cases performed emergently with a postoperative diagnosis of peptic ulcer disease were extracted. Using SPSS, correlations were then derived between patient factors, postoperative complications, and survival. P-values <0.01 were considered significant.
Results:
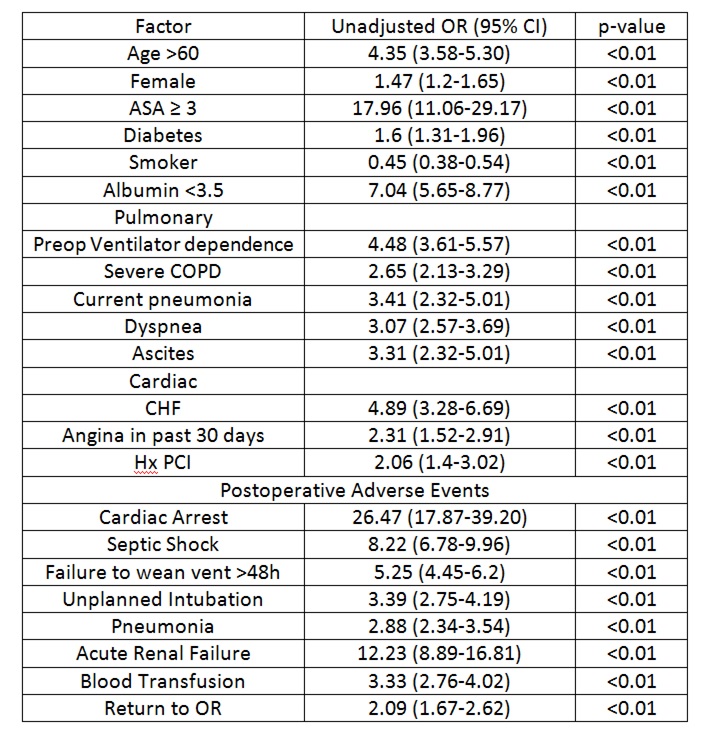
We extracted 5666 emergent cases with a postoperative diagnosis of perforated PUD. There were 723 deaths yielding a 30 day mortality rate of 12.8%. The mean age of the study population was 61. The most frequent postoperative complications were failure to wean from the ventilator within 48 hours (19.3%), need for blood transfusion (12.2%), septic shock (9.8%), and return to the operating room (9%). Non-survivors were more likely to be female, older, have a higher ASA classification, be functionally dependent and receive surgical treatment later within the hospital stay (Table 1). Females were more likely to be older, malnourished and receive transfusions despite a similar incidence of postoperative complications when compared to males. In a multinomial logistic regression model the patient factors with the highest risk for mortality were post-operative cardiac arrest (OR 13.7, 95% CI 7.4-25.3), septic shock (OR 4.1, 95% CI 2.9-5.7) and renal failure (OR 3.9, 95% CI 2.4-6.6).
Conclusion:
According to the NSQIP database, the mortality rate for emergent operations in perforated peptic ulcer disease was 12.8% which is consistent with prior studies. Older and female patients are at higher risk of death. This disease process appears to concentrate among older patients with a median population age of 61. Earlier diagnosis and surgical intervention improves survival. Poor nutritional status and certain post-operative complications may decrease the likelihood of survival.