F. Ali1, A. Dua1, S. Desai2 1Medical College Of Wisconsin,General Surgery,Milwaukee, WI, USA 2Southern Illinois University,Vascular Surgery,Springfield, IL, USA
Introduction: This study aims to investigate regional variations of outcomes including length of hospital stay, mortality and in-patient costs associated with patients undergoing pancreaticoduodenectomy in the United States.
Methods: A retrospective analysis was completed using the Nationwide Inpatient Sample to select patients with pancreatic cancer that underwent pancreaticoduodenectomy between 2007 and 2011 in the United States. ICD-9 codes were used to identify disease and procedure. Demographics, inpatient mortality, length of hospital stay and in-patient costs across different regions of the United States were compared. A multinomial regression was completed to compare the outcomes amongst the various regions.
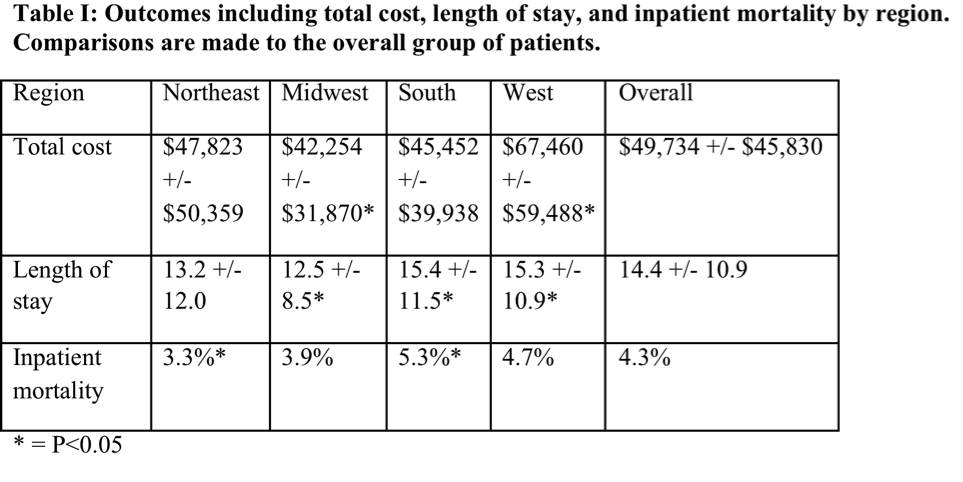
Results: A total of 27,267 pancreaticoduodenectomies for pancreatic cancer were performed in the United States during the five-year study period. There were no regional variations in demographics but in terms of comorbidities, COPD was significantly increased in the Midwest as compared to the Northeast (P<0.05), while renal failure was higher in the West compared to the Northeast (P<0.05). In terms of outcomes, length of stay was significantly higher in the South and West compared to the rest of the USA. The cost of care was also significantly higher in the west. Mortality rates were highest in the South (Table I).
Conclusion: Length of stay and mortality were highest in the South for patients undergoing Whipple procedures for pancreatic cancer whereas cost of care was highest in the West. There are no demographic variations within patient populations based on regions however patients in the West did have a higher incidence of renal failure which may contribute to the higher overall cost of in-patient care.