A. Shah2, A. Ashfaq2, S. R. Money2, C. K. Zogg1, J. Fraser4, V. J. Davila2, J. M. Chang2, T. Oyetunji3, R. J. Fowl2, W. Stone2, A. B. Chapital2, A. H. Haider1 1Brigham And Women’s Hospital,Center For Surgery And Public Health, Harvard Medical School, Harvard T H Chan School Of Public Health,BOSTON, MA, USA 2Mayo Clinic In Arizona,Department Of Surgery,Phoenix, AZ, USA 3Children’s Mercy Hospital And Clinics,Department Of Surgery,Kansas City, MO, USA 4Phoenix Children’s Hospital,Department Of Surgery,Phoenix, AZ, USA
Introduction:
Despite their rarity in the pediatric population, traumatic aortic injuries can prove to be highly lethal. Endovascular aortic repair (EVAR) has been successfully employed in the management of adult blunt aortic trauma. However, its efficacy has not been elucidated in the pediatric population. The objective of this study was to gauge the burden of traumatic aortic injuries using a nationally representative sample and compare outcomes associated with reparative modalities in a nationally representative population of adolescent patients.
Methods:
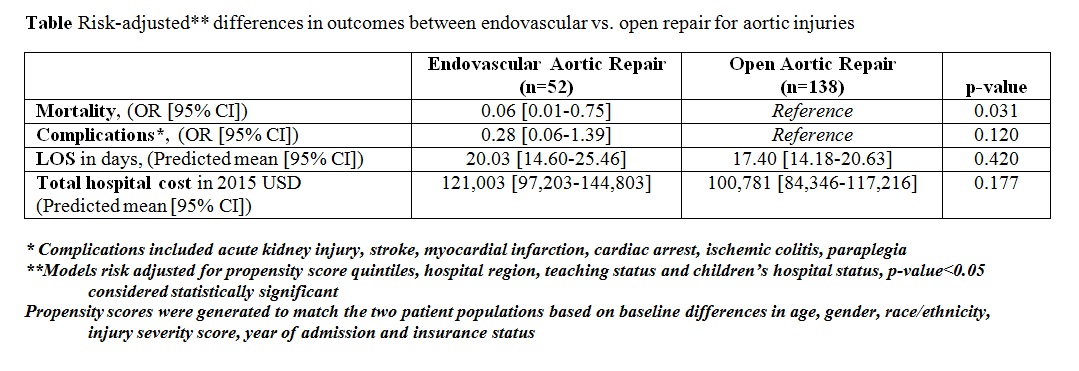
Four years (2000/2003/2006/2009) of data from the Kids Inpatient Database were queried for adolescent (10-19y) patients with diagnoses of blunt traumatic injuries to the abdominal/thoracic aorta. Included patients were divided into those who underwent EVAR and open aortic repair (OAR). Differences in associated outcomes — mortality, morbidity (acute kidney injury, stroke, myocardial infarction, cardiac arrest, ischemic colitis, paraplegia), length of stay (LOS), and total hospital cost of care — were compared using multivariable logistic/linear (family gamma; link log) regression. Propensity-score quintiles were used to account for differences in patient-level factors; models were further risk-adjusted to account for potential confounding associated with hospital region, teaching status, and children’s-hospital status. They were weighted to provide national estimates and account for clustering of patients within hospitals.
Results:
A total of 161 records were identified, weighted to represent 244 admissions nationwide. Average age on presentation was 17.0 (±2.0y) with a male preponderance (75.6%). EVAR was attempted in 27.4% (n=52) of cases. Patients who underwent EVAR had higher median ISS compared to the OAR group (38 vs 33, p=0.002). Risk-adjusted odds of death among EVAR patients were significantly lower relative to patients managed using OAR (p=0.031). No differences were found for complications. Marginally significant differences were reported for both LOS and total cost of care (table). Relative to OAR patients, use of EVAR was associated with a risk-adjusted predicted mean difference of 2.6 additional days and a corresponding increase in cost of approximately $20,200.
Conclusion:
Despite higher ISS among adolescent patients undergoing EVAR procedures, risk-adjusted odds of death were significantly lower relative to OAR. Combined with a lack of variation in morbidity, the results suggest that EVAR is comparatively safe may even convey a survival advantage among adolescent patients. Ongoing research is needed to consider longer-term outcomes in a larger group of patients.