K. M. Caldwell1, L. R. Putnam1,2, S. Covey1, M. Diffley1, A. Hildebrandt1, A. Minzenmayer1, K. T. Anderson1,2, A. L. Kawaguchi1,2, K. P. Lally1,2, K. Tsao1,2 2Children’s Memorial Hermann Hospital,Pediatric Surgery,Houston, TX, USA 1University Of Texas Health Science Center At Houston,Pediatric Surgery,Houston, TX, USA
Introduction: Teamwork and effective communication are principles of safe patient care, especially in surgery. Distractions in the operating room can impair and/or interrupt these hallmarks as well as increase surgeon stress and fatigue, potentially compromising patient safety. However, little is known about the type and frequency of distractions in operating rooms. We aimed to characterize interruptions in pediatric operating rooms in order to identify areas for intervention.
Methods: Over an eight week period, a prospective, direct observational study was performed by five trained observers in an academic children’s hospital. Convenience sampling was performed across all pediatric surgical specialties. The number of phone calls, people entering, pages/text messages, equipment failures, and other events that interrupted workflow were recorded. Interruptions were further defined as essential or non-essential based on their contribution to patient care. Interruptions were analyzed in relation to surgical subspecialty and case duration.
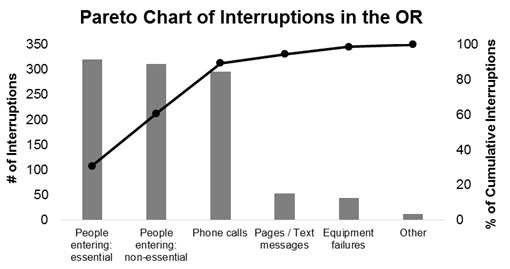
Results: 208 operations were observed with a median (interquartile range) operating time of 40 (19-86) minutes. A total of 1,037 interruptions were recorded with a median of 2 (1-5) interruptions per case. People entering the operating room accounted for the highest proportion of interruptions (61%), where approximately one-third were non-essential (30.5%). Overall, 64% of all the interruptions were non-essential to patient care (Figure). In total, 63% of the operations had at least one non-essential interruption. Interruptions were more frequent as case length increased (median per case; <30 min = 1, 31-60 min = 2, 61-120 min = 4, >121 min = 14).
Conclusion: Non-essential interruptions are common in pediatric operating rooms. The impact of these distractions on patient safety remains unknown. Although no single interruption was observed to cause direct patient harm, patient safety in the operating room may be optimized through awareness, education, and limiting non-essential interruptions. Future interventions should target eliminating non-essential interruptions and minimizing essential ones through prevention and process improvement.