M. A. Wasserman3, J. M. Sternbach3, M. W. Wandling3, M. L. Crandall1,3, N. M. Issa1,3, S. J. Schwulst1,3, K. Y. Bilimoria2,3, M. B. Shapiro1,3, M. Swaroop1,3 1Northwestern University,Department Of Trauma & Critical Care,Chicago, IL, USA 2Northwestern University,Surgical Outcomes And Quality Improvement Center,Chicago, IL, USA 3Northwestern University,Department Of Surgery,Chicago, IL, USA
Introduction:
Despite a lack of scientific evidence, obtaining multiple daily arterial blood gas (ABG) values on non-septic mechanically ventilated patients is commonplace in our Surgical Intensive Care Unit (SICU). Invasive arterial sampling has inherent risks to patients, and frequently may be replaced with less invasive monitoring tools. We aim to decrease ABG utilization for ventilatory monitoring by increasing the use of non-invasive end-tidal CO2 (ETCO2) monitoring.
Methods:
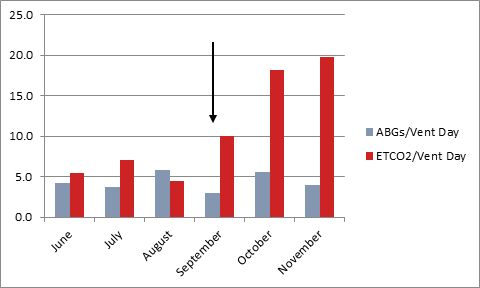
Through multidisciplinary meetings, educational materials were developed and distributed to all SICU healthcare providers, including nursing staff, respiratory therapists, and surgical residents. This education focused on appropriate ABG utilization, the capabilities of ETCO2 monitoring in managing mechanically ventilated patients, and the practical functionality of the ETCO2 devices. On September 1, 2014 a protocol mandating ETCO2 monitoring for all ventilated patients was implemented in the SICU. Using our institution’s Enterprise Data Warehouse, ABG and ETCO2 monitor utilization data was collected for three months preceding and three months following our intervention.
Results:
Prior to our educational intervention, 5.63 ETCO2 monitor recordings were documented per ventilator-day. Post-intervention, 16.0 ETCO2 recordings per ventilator-day were recorded. This difference was statistically significant (p<0.01) and represented a nearly three-fold increase in ETCO2 monitoring. There was a trend towards decreased ABG utilization following our intervention, though this did not meet statistical significance (4.62 pre-intervention vs. 4.13 post-intervention, p=NS).
Conclusion:
The increase in ETCO2 utilization following our intervention represents the first step in a culture shift away from considerable reliance on ABG values for routine ventilatory monitoring and toward a less invasive monitoring practice. Though there was a trend towards decreased ABG utilization following intervention, failure to reach statistical significance likely reflects a lack of comfort among providers in rapidly abandoning an ingrained practice.