S. P. Lawrence1,2, E. M. Hechenbleikner1,2, S. Cane3, L. Boyle1,3, W. B. Al-Refaie1,2,3 1Georgetown University Medical Center,Washington, DC, USA 2MedStar Georgetown Surgical Outcomes Research Center,Washington, DC, USA 3MedStar Georgetown University Hospital,Washington, DC, USA
Introduction: Surgical time-outs have been implemented in operating rooms (OR) to increase adherence to operative safety measures. Hospitals striving to become High Reliability Organizations must maximize safety protocol adherence and better understand sources of variability in heterogeneous OR settings. This study utilized a comprehensive auditing tool to analyze compliance and variation across the perioperative time-out process in a major metropolitan academic medical center.
Methods: Data were collected prospectively by 5 anonymous observers over 10 weeks. The auditing tool was developed by a multidisciplinary OR safety team with key stakeholders from anesthesiology, nursing, and surgery. The tool was a detailed checklist evaluating 3 phases of our time-out process: anesthesia, surgical (incision to closure), and debriefing (end of case before leaving the OR). The anesthesia time-out consisted of 7 criteria, the surgical consisted of 24 criteria, and the debriefing consisted of 10 criteria.
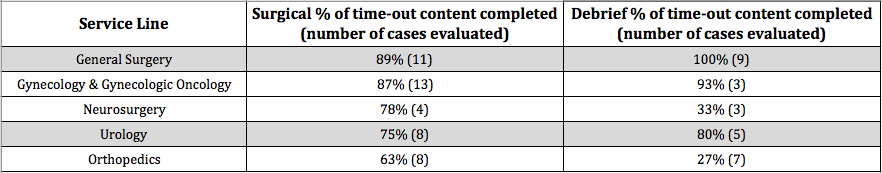
Results: In total, 111 time-outs were observed (anesthesia n=29, surgical n=50, and debriefing n=32). The time-outs were initiated during 50 OR cases across 24 surgeons within 7 surgical service lines. Across all service lines, the percentage of time-out content captured in anesthesia, surgical, and debriefing time-outs was 97%, 82%, and 71%, respectively. Between service lines, there were wide variations in the completion rate of surgical and debriefing time-outs (Table 1). Anesthesia time-outs were performed by an attending physician 86% of the time and occurred prior to induction in 97% of cases. Surgical time-outs were performed by an attending physician 98% of the time and occurred prior to draping in 96% of cases. Debriefing time-outs were always performed by an attending physician. Capture rates of surgical content varied from 16% (asking team members to call attention to any problems seen during the case) to 50% (asking team members to introduce themselves by name and role) to 62% (asking team members to address any special considerations during the case) and 100% (naming the procedure and patient information). Finally, within the debriefing time-out, the name of the procedure and reconciling the surgical tool counts were addressed in 84% of cases, while all other content was completed at or below the rate of the debriefing taking place (69%).
Conclusion: This perioperative auditing tool discovered wide variation in protocol adherence between surgical service lines. This practical checklist will be the basis for future designed interventions to target specialty-specific areas of need to ensure patient safety and surgical team cohesiveness in the operating room.