B. Styskel1, B. Wernick1, R. N. Mubang1, D. M. Sabol1, M. A. Granson1, J. C. Rosenfeld1, S. D. Moffatt-Bruce2, S. P. Stawicki1 1St. Luke’s University Health Network,Department Of Surgery,Bethlehem, PA, USA 2Ohio State University,Department Of Surgery,Columbus, OH, USA
Introduction: Despite tremendous technological and organizational progress over that last three decades, patient safety experts continue the struggle to eliminate ‘never events’. Among the most dreaded surgical misadventures are retained surgical items (RSI). Difficult to intercept, a number of different surgical tools and accessories continue to be ‘left behind’, yet little is known about the natural history of patients who ultimately suffer the consequences of these surgical errors.
Methods: An exhaustive literature search identified a total of 281 case reports and series describing 299 incidents of RSI between 1953 and 2015. All available details regarding each reported case were tabulated and standardized into the following categories: (a) demographics; (b) anatomic location of the retained object; (c) type of retained item; (d) time to identification/removal; (e) associated complications; and (f) pathology findings. Results are presented as descriptive statistics and frequencies.
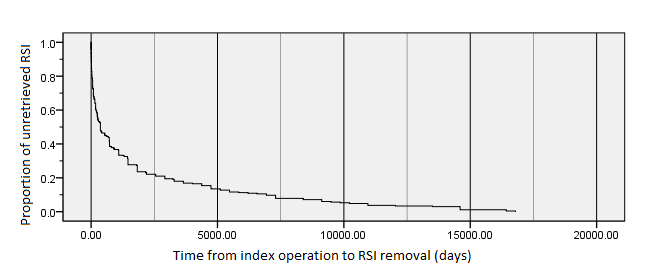
Results: A total of 299 RSI instances were tabulated. There were 107 males and 192 females, with average age of 47 years. The most common anatomic location was abdominal (113), paraspinal/spinal (33), thoracic (30), pelvic (28), cranial/facial (19), and extremity (12). Surgical sponge was the most common RSI type (180), followed by other types of gauze (64), plastic/tubing (14), surgical instrument (9), and needle (8). Median time to retrieval was 365 days (range, 0 to 16,790 days, 25%-75% IQR 60-1,825 days, Figure 1). Twenty-four cases (8%) involved 2 or more procedures. Almost all (281/299, 94%) objects were removed, and in 52 instances (17%) bowel or other organ resection was required. Median RSI-attributable hospital length of stay was 7 days. Significant complications were reported in 93/299 (31%) cases.
Conclusion: This collected series of RSIs provides an important glimpse into the natural history and patterns of occurrence of these ‘never events’. One in four patients had significant RSI-related complications, and the median length of stay attributable to RSI was 6 days. Majority of RSIs in this series were recognized and removed within 2 years of index operation, with the remainder either remaining asymptomatic and being discovered incidentally at a later time, or becoming symptomatic after a long period of dormancy. These findings corroborate and highlight the need for a national RSI registry.