C. Mosquera1, T. L. Fitzgerald1, E. E. Zervos1 1East Carolina University Brody School Of Medicine,Division Of Surgical Oncology,Greenville, NC, USA
Introduction: Pancreas resection is among the highest risk procedures in terms of post-operative mortality. The purpose of the study was to determine predictors and causes of early and late post-operative mortality in patients undergoing pancreatectomy.
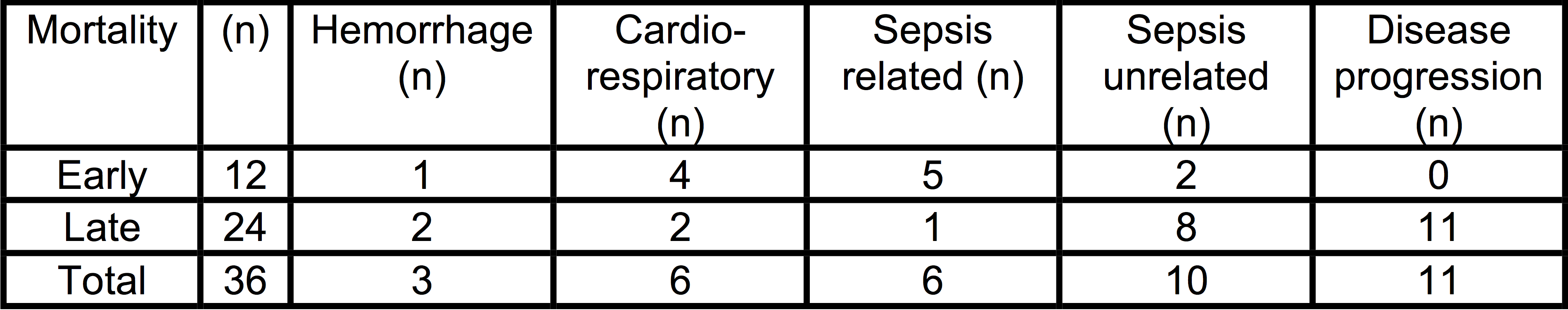
Methods: A prospective pancreas surgery registry at a very-large volume hospital was queried to identify early (30-day) and late (90-day) postoperative mortality between 2008 and 2015. Logistic regression was undertaken to determine predictors of each. Causes of death were categorized as: hemorrhagic, cardiorespiratory, sepsis and disease progression. Sepsis was sub-categorized as related (presence of infected intra-abdominal collections, abscess, fistula, and surgical site infection) or unrelated to surgery (pneumonia, CLABSI, CAUTI). Disease progression signified withdrawal of care in an otherwise viable patient due to perceived poor prognosis as a result of documented recurrent or persistent disease.
Results: A total of 312 patients underwent resection (68% Whipple, 32% Distal Pancreatectomy). Early postoperative mortality occurred in 12 (3.8%) patients and late in 24 (7.7%) patients with a total postoperative mortality of 11.5%. Early deaths occurred during index admission in 83% while 95.5% of late deaths occurred outside of the hospital or in patients that were discharged and returned to hospital and died. (Table)
On univariate analysis, age, smoking history, intensive care unit requirement (ICU), presence of complications, operative estimated blood loss, body mass index, discharge destination, presence of tachycardia, elevated WBC at discharge and type of insurance predicted any postoperative mortality. On multivariate analysis, only ICU (OR 20.3 p 0.0003) and discharge destination of home and SNF compared to rehabilitation facility remained significant (p<0.05). Private insurance was a protective factor compared to Medicare, Medicaid and uninsured (p<0.05). Sepsis arising from surgical complications was the primary source of early postoperative mortality while disease progression was the most common cause of late mortality.
Conclusion: Surgical complications remain the primary source of early postoperative mortality, which are largely unavoidable. Late postoperative mortality may be mitigated by minimization and early detection of hospital-acquired infection through adherence to best care guidelines and neo-adjuvant strategies to identify patients with low risk of disease progression in which further treatment is non futile.