J. S. Park1, Y. Nakache4, J. Katz3, R. D. Boutin3, A. Monjazeb2, R. J. Canter1 1University Of California – Davis,Surgical Oncology,Sacramento, CA, USA 2University Of California – Davis,Radiation Oncology,Sacramento, CA, USA 3University Of California – Davis,Radiology,Sacramento, CA, USA 4University Of California – Davis,Medical School,Sacramento, CA, USA
Introduction:
Desmoid tumors are locally aggressive neoplasms without metastatic potential. Although surgical resection was once thought to be the mainstay of therapy, this is a potentially morbid approach associated with a high risk of local recurrence. There is an increasing role for watchful waiting and conservative management for these tumors.
Methods:
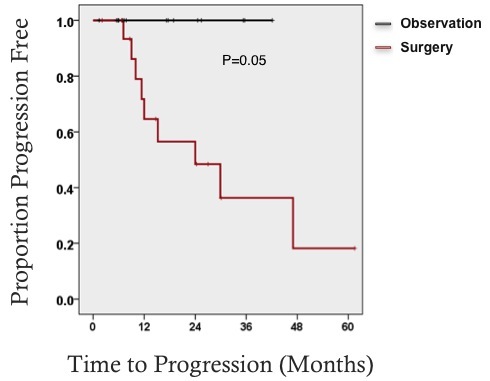
We identified 36 desmoid tumor patients who were categorized by the nature of treatment rendered (surgical resection versus observation). Data were abstracted on clinical and pathological factors. Disease stability or progression was determined radiographically. Univariate and Kaplan-Meier analysis was used to determine predictors of recurrence/progression of disease. Main outcome measurements were tumor recurrence following surgical resection versus tumor progression with conservative management.
Results:
Of the 36 patients, 58% were female and average age was 44 years old. The tumors were primarily located in the extremities including hip and shoulder girdle at 58%. 33% were located in the trunk and 8% in the retoperitoneum. Median tumor size was 9.2 cm (range 2.7-24 cm). Of the patients that had beta catenin staining, 96% were positive. The patients were categorized into surgical versus nonsurgical therapy. 18 patients underwent operation either prior to referral, due to refractory symptoms or due to patient preference. 17 patients were observed without surgical resection, including 3 patients who received nonsurgical therapy such as chemoradiation and/or medical therapy. One patient was lost to follow up. Median follow up time was 23 months.
Among 17 of the patients who underwent surgical resection, ten patients developed recurrent disease (59%). Among those who developed recurrent disease, 8 (80%) patients were stable or partially responding to subsequent observation. Of the 17 patients who underwent conservative management, one patient experienced disease progression (5%) and 94% of patients had no disease progression, including one patient with complete response and three patients with partial responses.
Conclusion:
This retrospective analysis adds to growing data that observation of both primary and recurrent desmoid tumors is safe and effective with higher rates of stable disease than other published series. Conservative management of desmoid tumors appears to be safe and effective, sparing patients the morbidity and risk of recurrence that is associated with extensive operations.