S. X. Jin1, T. W. Yen1, A. A. Carr1, B. Lalande1, K. Doffek1, D. B. Evans1, T. S. Wang1 1Medical College Of Wisconsin,Surgical Oncology/Surgery,Milwaukee, WI, USA
Introduction: Frailty, defined as decreased physiologic reserves due to decline of multiple organ systems, is a risk factor for poorer postoperative outcomes in the elderly. Cervical endocrine surgery (thyroidectomy and parathyroidectomy) is associated with low rates of morbidity and mortality, and is increasingly being performed in the elderly. This study sought to identify potential frailty biomarkers in patients undergoing cervical endocrine surgery.
Methods: A retrospective chart review of prospective databases was performed of 309 patients who underwent thyroidectomy and/or parathyroidectomy between 7/1/2012 to 6/30/2013. Demographic and clinical data were collected, including pre- and postoperative lab values, extent of surgery, length of stay (LOS) and postoperative complications within 30 days of surgery. Endocrine-specific complications were documented for 6 months in order to categorize transient vs. permanent injury; patients with <6 months of follow-up were not excluded from the cohort. Patients were divided into groups by age: <50, 50-64, and ≥65 years. Finally, to identify potential frailty markers, preoperative biochemical data were compared between patients who experienced complications and those who did not. Kruskal-Wallis test was used for continuous variables and chi-squared test was used for categorical data; a p-value <0.05 was considered statistically significant.
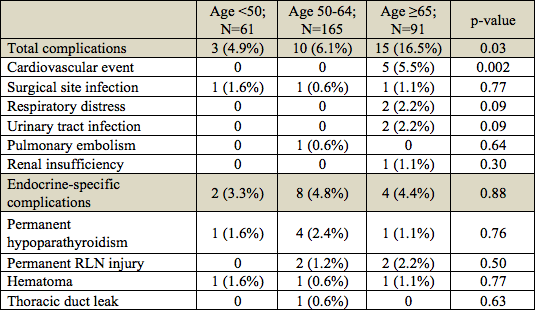
Results: Median age was 57 years (range, 19-86) and 252 (82%) patients were female. The median LOS was one day, and there was no difference in LOS among the three age groups (p=0.87). Overall, there were 28 complications; 14 (50%) were endocrine-specific (Table 1). Patients ≥65 years experienced more complications (n=15; p=0.03) overall and more cardiac events (n=5; p=0.002) than patients 50-64 and patients <50 years. There was no difference in endocrine-specific complication rates by age group. When analyzed by preoperative biochemical values and comorbidities, there were no biochemical factors that were associated with the development of complications. However, patients who experienced complications had a higher rate of anticoagulant use (22% vs. 5%; p=0.001) and congestive heart failure (CHF) (9% vs. 2%; p=0.03), compared to those who did not.
Conclusion: In this cohort, age correlated with higher postoperative complications but was not predictive of hospital LOS. Preoperative factors such as anticoagulant use and history of CHF may be markers for frailty in cervical endocrine patients.